Chronic pain isn’t just a symptom-it’s a whole new way of living.
When pain sticks around for more than three months, it stops being a warning sign and starts becoming your daily reality. For 50 million adults in the U.S. alone, chronic pain means waking up with stiffness, moving through the day with tension, and going to bed wondering if tomorrow will be any better. It’s not just in the back, the knees, or the nerves-it’s in the mind, the job, the relationships, and the sleep. The old idea that pain means damage and needs a pill to fix it? That’s outdated. Today’s science says something very different: chronic pain is a complex condition that responds best to a mix of movement, mindset, and support-not just medicine.
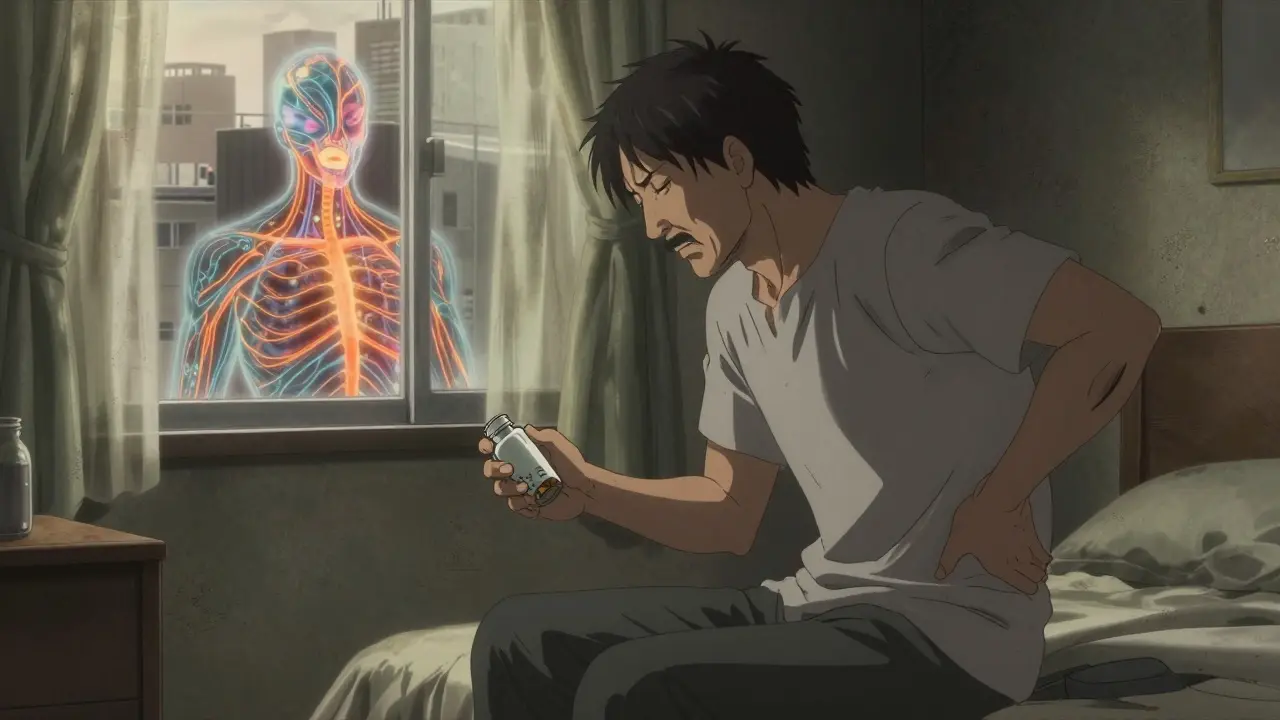
Why pills alone don’t work long-term
Opioids were once the go-to for chronic pain. But the data now shows they don’t hold up. After three to six months, most people get little extra pain relief, while the risks keep climbing. The CDC found that people taking more than 50 morphine milligram equivalents (MME) per day have a 40% higher chance of overdose. And yet, even after the 2022 CDC guidelines warned against routine opioid use, only 5% more patients were referred to non-drug treatments. That gap tells you something: doctors want to help, but they’re often stuck with outdated tools and no time to offer better options.
Meanwhile, non-opioid painkillers like ibuprofen or acetaminophen help for flares, but they don’t fix the deeper problem. Long-term use can damage your stomach, liver, or kidneys. And drugs like pregabalin or duloxetine? They work for some, but side effects like dizziness or weight gain make them hard to stick with. The truth? Medications have a role-but only as part of a bigger plan.
The power of movement-no gym membership needed
One of the most proven ways to reduce chronic pain is to move. Not to push through pain, but to move in ways your body can handle. Studies show that structured exercise programs lasting 6 to 12 weeks, done 2-3 times a week, can cut pain by 15-30% and improve daily function by 20-40%. You don’t need to run marathons. Walking, swimming, tai chi, yoga, or even gentle resistance training with bands can rebuild strength and calm the nervous system.
Why does this work? Chronic pain often makes your body hypersensitive. Movement teaches your brain that motion isn’t dangerous. A 2023 guide from Northwest PA Injury Guidance recommends starting slow: 10 minutes a day, three times a week. Build up gradually. Track how you feel-not just pain levels, but energy, sleep, and mood. Many people report that after six weeks, they’re doing things they hadn’t done in years: playing with grandkids, gardening, walking to the store without fear.

Cognitive Behavioral Therapy: Rewiring your brain’s pain response
If you’ve ever heard someone say, “It’s all in your head,” they meant it the wrong way. Chronic pain isn’t imaginary-but your brain’s reaction to it can be changed. Cognitive Behavioral Therapy (CBT) isn’t about positive thinking. It’s about learning how your thoughts, emotions, and behaviors feed into pain. A typical CBT program for pain includes 8-12 weekly sessions, each 50-90 minutes long. You learn to spot catastrophic thoughts like “I’ll never get better” or “This pain means I’m broken,” and replace them with more helpful ones: “I can manage this flare,” or “My body is healing, even if it’s slow.”
The results? Studies show CBT reduces pain intensity by 25-40%, cuts disability by 30%, and slashes pain-related anxiety by up to 50%. One veteran shared in a VA report that after 12 sessions, he dropped his daily opioid dose from 120 MME to 30 MME-and started walking his dog again. That’s not luck. That’s science.
The gold standard: Multidisciplinary pain programs
When pain becomes all-consuming, single treatments often fall short. That’s where multidisciplinary rehabilitation programs come in. Think of them as pain boot camps. The Mayo Clinic’s three-week intensive program brings together doctors, psychologists, physical therapists, occupational therapists, and counselors-all working as a team. Patients learn biofeedback, stress control, pacing techniques, and how to rebuild daily routines without relying on painkillers.
The outcomes? Sixty to seventy-five percent of participants report major improvements in function. Half of them reduce or quit opioids entirely. And 60-75% go back to work or meaningful daily activities. These programs don’t promise to erase pain. They promise to help you live well despite it. The catch? They’re hard to access. Only 15-20% of people who could benefit actually get in. Costs run $15,000-$20,000 per person, and insurance often denies coverage-even though guidelines say these programs work.

What’s holding people back?
There’s a big gap between what science says and what patients actually get. A 2023 Health.mil survey found 68% of chronic pain patients struggled to find providers trained in non-drug approaches. On Reddit’s r/ChronicPain, 72% of comments said their doctor offered either opioids or nothing. Insurance companies still routinely deny coverage for CBT, physical therapy, or acupuncture-even when guidelines recommend them. And for Black patients, the problem is worse: a 2023 JAMA study showed they’re 40% less likely to receive evidence-based non-drug care, even when their pain levels are the same as white patients.
Financial barriers are huge. Therapy sessions cost $100-$150 each. Acupuncture isn’t covered everywhere. Even walking shoes and resistance bands add up. For people on fixed incomes or without paid time off, trying to attend weekly appointments feels impossible.
What’s changing-and what’s next
Change is coming, but slowly. Medicare expanded coverage for non-drug pain treatments in 2023. The NIH has poured $1.8 billion into research for non-addictive pain therapies, with 12 new drugs in late-stage trials. Wearable devices like Nevro’s Senza and Boston Scientific’s Wave are now FDA-approved and can reduce pain by 30-40% through nerve stimulation. Digital tools like reSET-O, a prescription app for opioid use disorder, are helping people track progress and stay on track.
But real progress needs more than tech. It needs trained providers, fair insurance rules, and better access in rural areas where 65% of counties have no pain specialist. It needs doctors who take time to listen. It needs patients who know they deserve better than a prescription and a shrug.
Where to start today
You don’t need to wait for the system to fix itself. Here’s what you can do now:
- Ask your doctor for a referral to a physical therapist who specializes in chronic pain-not just injury rehab.
- Look for a CBT therapist trained in pain management. The American Chronic Pain Association has a directory.
- Start moving, even if it’s just 10 minutes of walking or stretching daily. Track your progress in a notebook.
- Join a support group. Whether online or in person, sharing with others who get it reduces isolation.
- Ask about your insurance coverage for non-drug treatments. If denied, appeal. Many denials are overturned with the right documentation.
Chronic pain doesn’t have to be your whole identity. It’s a challenge, yes-but it’s not the end of your life. With the right tools, people rebuild careers, relationships, and joy. It takes effort. It takes time. But it’s possible.
Is chronic pain the same as acute pain?
No. Acute pain is a short-term signal that something is injured-like a sprained ankle or surgery. It usually fades as the body heals, within days or weeks. Chronic pain lasts longer than three months, even after the original injury has healed. It’s no longer about tissue damage; it’s about how the nervous system has changed and become oversensitive. That’s why treatments for acute pain (like rest and painkillers) often don’t work for chronic pain.
Can I stop taking opioids if I’ve been on them for years?
Yes, but it needs to be done carefully. Stopping suddenly can cause withdrawal and make pain worse. Work with a doctor who understands tapering strategies. Many people successfully reduce or stop opioids by combining gradual dose reduction with non-drug treatments like CBT, exercise, and mindfulness. The CDC recommends monthly check-ins to assess risks and benefits. Some patients reduce their dose by 10% every 2-4 weeks, while others need longer. The goal isn’t just to quit pills-it’s to improve your life without them.
Does acupuncture really help with chronic pain?
It depends on the condition. For osteoarthritis of the knee or chronic low back pain, studies show acupuncture reduces pain by 20-30% more than fake treatments. But for nerve pain (like diabetic neuropathy), the benefits are small or nonexistent. It’s not a cure, but it can be a helpful tool for some people, especially when combined with other therapies. Look for licensed practitioners and check if your insurance covers it.
Why do some doctors still push opioids for chronic pain?
Many doctors were trained in the 1990s and early 2000s when opioids were seen as safe and effective. Some still believe they’re the easiest solution, especially under time pressure. Others fear losing patients if they don’t prescribe. But guidelines have changed since 2016, and most major medical groups now say opioids should be a last resort. If your doctor doesn’t offer alternatives, ask for a referral to a pain specialist or ask about the CDC’s guidelines. You have the right to ask for evidence-based care.
What if I can’t afford therapy or a pain program?
Cost is a real barrier, but there are options. Look for community health centers that offer sliding-scale fees. Some universities with psychology or physical therapy programs run low-cost clinics staffed by supervised students. Online CBT programs like This Way Up or PainCourse are affordable and evidence-based. Free resources like the American Chronic Pain Association’s website offer guided exercises, journaling tools, and peer support. Movement doesn’t cost money-start with walking, stretching, or breathing exercises. Small steps add up.






Nick Flake
February 3, 2026 AT 09:40