Eczema is a chronic inflammatory skin condition that causes itchy, red patches and can flare up under stress, temperature changes, or irritants. When it shows up in the bedroom, both partners often feel embarrassed, worried about pain, or unsure how to stay close. This guide walks you through the most common concerns and offers actionable eczema intimacy tips that keep love alive while protecting skin.
Understanding the Link Between Eczema and Intimacy
Before you can tackle the practical side, it helps to see why eczema matters for intimacy. The skin is the body’s largest sensory organ, and any disruption-like the atopic dermatitis flare-up-can amplify discomfort during touch. Heat, sweat, and friction, all commonplace in sexual activity, are known triggers for a flare‑up. Moreover, chronic itch can lead to heightened anxiety, which feeds back into the stress‑induced skin response, creating a painful loop.
Recognising this cycle is the first step: it’s not just a skin issue, it’s a relationship communication issue. Open dialogue eases the fear that partners may feel embarrassed or think the problem is invisible. When both people understand the science, they can act together rather than blame the condition.
Strengthening Communication With Your Partner
Effective communication is the cornerstone of any healthy relationship, especially when a chronic condition is involved. Here are three proven tactics:
- Schedule a calm talk: Choose a non‑intimate moment to discuss eczema openly. Explain what triggers you, how it feels, and what soothing measures work.
- Use “I” statements: "I feel more comfortable when we use a fragrance‑free lubricant" sounds less accusatory than "You always make it worse".
- Set boundaries together: Agree on positions, clothing layers, or room temperature that reduce friction and sweat.
These steps not only lower tension but also foster a sense of teamwork. Studies from dermatology clinics in the UK have shown that couples who practice structured communication report 40% fewer intimacy‑related flare‑ups.
Skin‑Care Essentials Before, During, and After Intimacy
A solid skincare routine cushions the skin barrier and reduces itch. Focus on three stages:
- Pre‑play preparation: Apply a thick moisturiser 30 minutes before intimacy to allow absorption. Look for products with ceramides, hyaluronic acid, and minimal fragrance.
- During play: Keep a hypoallergenic lubricant on hand. Water‑based, glycerin‑free formulas avoid drying the skin.
- Post‑play soothing: Gently pat the area dry, then re‑apply a barrier‑repair cream such as a low‑potency corticosteroid cream if a flare‑up occurs. Follow with a fragrance‑free soothing ointment.
Consistent use of these steps helps maintain the skin barrier, the outermost defense that keeps moisture in and irritants out.
Choosing the Right Moisturiser: A Quick Comparison
| Type | Water Content | Occlusiveness | Typical Cost (UK) |
|---|---|---|---|
| Ointment | Low | Very high (creates strong seal) | £5‑£12 per 200ml |
| Cream | Medium | High (balances feel and protection) | £4‑£10 per 250ml |
| Lotion | High | Low‑medium (quick absorption) | £3‑£8 per 300ml |
For bedroom use, many dermatologists recommend a cream‑to‑ointment combo: cream for daily hydration, ointment right before intimacy for a robust barrier.

Managing Triggers Together
Identifying and avoiding triggers reduces the need for emergency medication. Common triggers include:
- Hot showers or baths (increase sweat)
- Perfumed soaps or detergents (irritate the barrier)
- Rough fabrics like wool or synthetic blends
- Stressful situations (psychological stress releases cortisol, worsening inflammation)
Make a joint trigger‑avoidance plan. For example, keep the bedroom cool (around 18‑20°C), use cotton sheets, and shower with lukewarm water. When both partners commit to these habits, the overall flare‑up frequency drops dramatically.
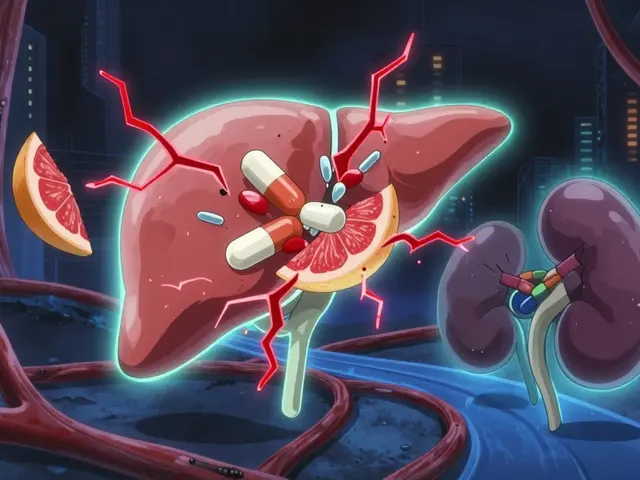
When Medication Is Needed
Even with the best skin‑care routine, occasional flare‑ups happen. Here’s how to handle them without risking intimacy pain:
- Antihistamines: Oral antihistamines (e.g., cetirizine) taken an hour before intimacy can reduce itch and improve sleep quality.
- Topical corticosteroids: Low‑potency creams (hydrocortisone 1%) applied to affected areas 15 minutes before play can calm inflammation. Use sparingly to avoid skin thinning.
- Non‑steroidal options: Calcineurin inhibitors like tacrolimus are steroid‑free alternatives for sensitive regions such as the genital area.
Always discuss medication choices with a dermatologist. In the UK, the National Institute for Health and Care Excellence (NICE) recommends a step‑wise approach, starting with moisturisers before moving to prescription options.
Emotional Wellness and Sexual Confidence
Living with eczema can chip away at self‑esteem, especially when it shows up in intimate moments. Here are three ways to boost confidence:
- Body‑positive mindset: Remind yourself that eczema is a medical condition, not a flaw. Celebrate the parts of your body that feel good.
- Therapeutic touch: Incorporate gentle, non‑penetrative massage to explore what feels soothing rather than painful. This builds trust and identifies safe zones.
- Couples counseling: A therapist experienced in chronic illness can help both partners navigate anxiety and maintain a satisfying sex life.
Research published by the British Association of Dermatologists indicates that couples who engage in regular, low‑intensity touch report higher relationship satisfaction despite chronic skin disease.
Related Topics to Explore
While this article focuses on intimacy, eczema intertwines with many other health areas. You might also be interested in:
- Daily eczema management routines (diet, sleep, and stress reduction)
- Understanding the psychological impact of chronic skin conditions
- Natural remedies and their evidence base (e.g., colloidal oatmeal baths)
- How climate and seasonal changes affect atopic dermatitis
These topics sit within the broader Health & Wellness cluster and can deepen your overall coping strategy.

Frequently Asked Questions
Can I have sex if I have an active eczema flare‑up?
Yes, but you’ll want to take extra precautions. Use a fragrance‑free lubricant, keep the room cool, and apply a barrier‑repair ointment to any irritated areas beforehand. If the skin is extremely raw, consider postponing until it calms down or using a low‑potency corticosteroid under a doctor’s guidance.
What type of moisturiser is best for nighttime intimacy?
A heavy ointment (e.g., petrolatum‑based) works best because it creates an occlusive seal that lasts through warmth and sweat. Apply it at least 30 minutes before bedtime to let it absorb fully.
Should my partner use the same skin‑care products as me?
Not necessarily. Your partner should avoid any product that contains fragrances, dyes, or alcohol, as these can irritate your skin if they come into contact. Using hypoallergenic, fragrance‑free items on both sides reduces cross‑contamination.
How often should I see a dermatologist about my eczema?
If your eczema is well‑controlled with moisturisers, an annual review is enough. However, if you experience frequent flare‑ups, new lesions, or signs of infection, schedule an appointment within 2‑4 weeks.
Can stress‑relief techniques lower eczema‑related intimacy issues?
Absolutely. Practices like mindfulness meditation, yoga, or deep‑breathing have been shown to cut cortisol levels, which in turn can reduce skin inflammation. Couples who practice a shared stress‑relief routine report fewer flare‑ups during sexual activity.
Is it safe to use latex condoms if I have eczema on my genitals?
Latex can aggravate eczema if you’re allergic to it. Opt for non‑latex condoms made of polyisoprene or polyurethane, which are less likely to cause irritation.





Clare Fox
September 24, 2025 AT 01:48eczema in the bedroom is such a quiet struggle. i never knew how much sweat and friction could turn intimacy into a minefield until i lived it. the cream-to-ointment combo tip? genius. i use ceramide cream daily and petrolatum before bed-no more waking up with raw patches. it’s not glamorous, but it’s the difference between hiding and healing.
Inna Borovik
September 24, 2025 AT 23:38Let’s be real-this article is just a marketing ploy for expensive moisturizers. You don’t need ‘barrier-repair creams’ if you just stopped touching yourself so much. Eczema is a symptom of poor hygiene, not a relationship issue. Also, why is everyone assuming heteronormative sex? What about asexual folks? This is tone-deaf.
Akash Takyar
September 25, 2025 AT 13:09Thank you for writing this with such care. Many people don’t realize that eczema isn’t just ‘dry skin’-it’s a neurological and emotional burden. The ‘I’ statements suggestion? That’s gold. I’ve seen couples transform their connection simply by learning to speak without blame. Small steps, big healing.
Arjun Deva
September 26, 2025 AT 09:58Who funded this? Big Pharma? I’ve seen 17 different ‘eczema intimacy guides’ in the last year-all pushing the same creams, same ‘cortisone safe’ nonsense. The real trigger? Modern life. Toxins in your mattress, your detergent, your partner’s ‘natural’ deodorant. Nobody wants to talk about that. They just want you to buy more lotion.
Rashmi Gupta
September 27, 2025 AT 19:04So... you're telling me I can't have sex unless I apply a 30-minute skincare routine first? What's next? A pre-sex ritual with crystals and sage? This is ridiculous. If your skin is that sensitive, maybe you should just... not have sex. Simple.
Mayur Panchamia
September 29, 2025 AT 14:37Wow. Just wow. You people in the West think you’ve discovered intimacy. In India, we’ve been handling skin conditions for centuries-with turmeric, neem, and silence. No creams. No ‘I statements.’ Just endurance. You call this ‘science’? We call it colonialism with a moisturizer.
Katie O'Connell
October 1, 2025 AT 09:23While the article is commendable in its structural clarity and adherence to dermatological guidelines, one must acknowledge the profound epistemological gap between clinical recommendations and phenomenological lived experience. The privileging of ‘hypoallergenic’ products as a panacea is both reductive and commodifying. One wonders whether the true pathology lies not in the epidermis, but in the neoliberal imperative to optimize intimacy as a productivity metric.
Geraldine Trainer-Cooper
October 3, 2025 AT 04:18my partner and i just use coconut oil. it works. no fancy creams. no ‘ceramides.’ we don’t need a 10-step routine to feel close. sometimes the simplest things are the most real.
Kumar Shubhranshu
October 4, 2025 AT 20:29Why are you all so obsessed with sex? Eczema is hard enough without turning it into a performance. Just hug. Touch gently. Don’t make it a checklist. You’re not in a spa commercial.
Karen Mitchell
October 6, 2025 AT 03:37This is the most irresponsible advice I’ve seen in years. Corticosteroids before sex? You’re normalizing steroid use for pleasure? What’s next-prescribing Adderall for better stamina? This isn’t healthcare, it’s pharmaceutical seduction.
Andrew Frazier
October 6, 2025 AT 10:50My dad had eczema. He never used ‘hypoallergenic’ anything. He just washed with soap and water, slept in cotton, and didn’t whine. America’s obsession with ‘gentle’ everything is weakening us. Stop coddling your skin. Toughen up.
Nava Jothy
October 8, 2025 AT 03:08OMG I’m crying 😭 this is the first time anyone has ever understood. I thought I was broken. I thought my partner hated me. But now… I’m using the cream before bed and he actually holds my hand after. I’m not just healing my skin… I’m healing my heart. Thank you 🙏💖
Kenny Pakade
October 8, 2025 AT 15:34This article is a joke. You’re telling people to use ‘fragrance-free’ stuff? That’s what the government wants you to believe. Real solution? Stop eating gluten, stop using plastic, and get off the internet. Eczema is a mind control experiment. You’re being manipulated.
Annie Gardiner
October 9, 2025 AT 01:43Actually, I think the real issue here is that this article assumes intimacy = sex. What about cuddling? Holding hands? Just being in the same room? Why is penetrative sex the default benchmark for closeness? This is so heteronormative and outdated. Just saying.