Fluconazole is an oral triazole antifungal that inhibits the enzyme lanosterol 14α‑demethylase, disrupting fungal cell‑membrane synthesis. It is widely used for systemic mycoses because of its good oral bioavailability (≈90%) and low toxicity profile. When doctors face Paracoccidioidomycosis -a chronic granulomatous infection endemic to rural Latin America-fluconazole often becomes the first‑line oral option for mild‑to‑moderate disease. This article walks you through the hallmark signs, diagnostic steps, therapeutic nuances and practical ways to keep the fungus at bay.
Understanding Paracoccidioidomycosis
Paracoccidioidomycosis, sometimes called South American blastomycosis, is caused by the dimorphic fungus Paracoccidioides brasiliensis. In the environment it lives as a mold, producing infective conidia that become yeast once they settle in human tissue. The disease primarily affects agricultural workers who inhale spores while handling soil or coffee beans.
Typical Symptoms and Clinical Stages
The infection can linger silently for months before symptoms appear. Early pulmonary signs mimic tuberculosis: dry cough, mild fever, and chest pain. As the disease progresses, mucocutaneous lesions-especially on the oral mucosa-develop, often described as painful, ulcerated plaques with a characteristic “mulberry” appearance. Lymphadenopathy, weight loss and skin nodules are also common. In severe cases, the fungus disseminates to the central nervous system, causing headaches, seizures or focal deficits.
How Paracoccidioidomycosis Is Diagnosed
Definitive diagnosis hinges on laboratory confirmation. Direct microscopy of sputum, tissue biopsy or ulcer exudate reveals the classic "pilot’s wheel" budding yeast. Serology (counter‑immunoelectrophoresis) remains useful, showing titres above 1:32 in active disease. Imaging-chest X‑ray or CT-often displays bilateral reticulonodular infiltrates, while MRI may uncover brain lesions in disseminated infection.
Why Fluconazole Is Chosen
Fluconazole’s pharmacokinetic properties make it attractive for outpatient care. After a standard loading dose of 400mg on day1, maintenance dosing ranges from 200mg to 400mg daily, depending on disease severity and site of infection. The drug penetrates well into the lungs, cerebrospinal fluid and skin, reaching therapeutic concentrations that suppress fungal growth.
Comparing the Main Antifungal Options
| Agent | Route | Typical Adult Dose | Efficacy (clinical cure%) | Common Adverse Events |
|---|---|---|---|---|
| Fluconazole | Oral | 200‑400mgdaily | 80‑85 | Headache, mild hepatotoxicity |
| Itraconazole | Oral | 200mgtwice daily (loading), then 400mgdaily | 85‑90 | GI upset, hepatotoxicity, drug‑drug interactions |
| AmphotericinB | IV | 0.7mg/kgdaily (deoxycholate) or 3‑5mg/kgdaily (liposomal) | 90‑95 | Nephrotoxicity, infusion‑related fever |
While AmphotericinB offers the highest cure rates, its intravenous requirement and renal toxicity limit use to severe or disseminated disease. Itraconazole is often preferred for moderate disease because of its higher tissue penetration, but its variable absorption and extensive cytochromeP450 interactions demand careful monitoring. Fluconazole balances ease of oral dosing with a relatively low side‑effect burden, making it the go‑to for many clinicians handling uncomplicated cases.
Designing a Fluconazole‑Based Treatment Regimen
Therapy generally begins with a loading dose of 400mg on day1, followed by 200mg-400mg once daily for at least 6months. Some experts extend treatment to 12months for patients with extensive pulmonary involvement or CNS disease. Therapeutic monitoring includes baseline liver function tests, then repeat checks at month1, 3 and 6. Serum fluconazole concentrations are rarely needed but can be measured in refractory cases.

Managing Side Effects and Drug Interactions
Fluconazole is well tolerated; the most frequent complaints are mild headache and transient nausea. Hepatotoxicity occurs in <5% of patients, usually reversible after discontinuation. Because fluconazole inhibits CYP2C9 and CYP3A4, it can raise levels of warfarin, oral hypoglycemics and certain statins. Clinicians should adjust doses or select alternative agents when possible.
Prevention Strategies in Endemic Areas
Primary prevention revolves around exposure reduction. Wearing N95 masks during soil‑disrupting activities, improving ventilation in barns and using wetting techniques to suppress dust can cut inhalation of conidia. Secondary prevention-preventing relapse after treatment-relies on completing the full antifungal course and performing periodic serology (every 3‑6months) for at least two years.
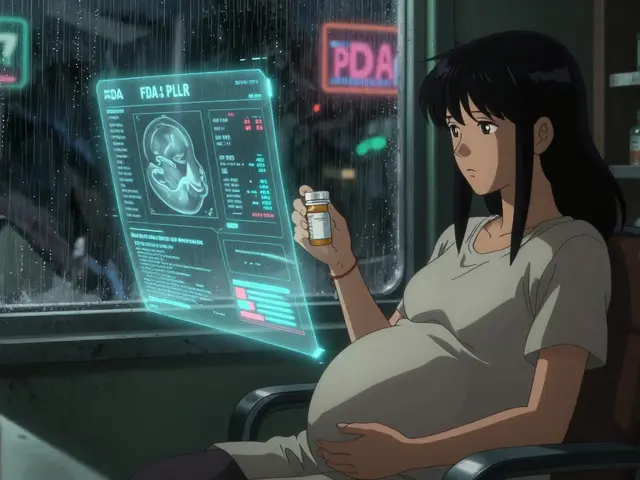
Special Populations: Children, Pregnant Women and Immunocompromised Hosts
In children, dosing is weight‑based (6mg/kgdaily) and generally well tolerated. Fluconazole is categoryC in pregnancy; low‑dose regimens (≤200mgdaily) may be used after risk-benefit discussion, but alternatives like amphotericinB are preferred during the first trimester. For HIV‑positive patients, drug‑drug interactions with antiretrovirals (especially protease inhibitors) are common; choosing a regimen that avoids CYP3A4 inhibition is critical.
Practical Checklist for Clinicians
- Confirm diagnosis with microscopy or serology.
- Assess disease severity and organ involvement.
- Start fluconazole: 400mg loading, then 200‑400mg daily.
- Baseline liver function; repeat at 1, 3, 6months.
- Screen for drug interactions (warfarin, statins, antiretrovirals).
- Educate patients on adherence and avoidance of dust exposure.
- Schedule serology follow‑up for 24months post‑therapy.
Related Topics You May Want to Explore
If you found this guide useful, you might also read about Chronic granulomatous disease, the role of antifungal stewardship in reducing resistance, and current WHO recommendations for neglected tropical mycoses.
Frequently Asked Questions
What makes fluoronazole suitable for treating paracoccidioidomycosis?
Fluconazole is highly bioavailable, penetrates lung and brain tissue, and has a relatively low side‑effect profile. These traits allow long‑term oral therapy, which is essential for a disease that can linger for months or years.
How long should treatment with fluconazole last?
For mild‑to‑moderate pulmonary disease, at least six months of daily dosing is recommended. More extensive disease, especially with CNS involvement, often requires 12months or longer, guided by clinical response and serologic trends.
Can fluconazole cause liver damage?
Mild elevations of liver enzymes occur in up to 5% of patients and are usually reversible after stopping the drug. Routine monitoring of ALT/AST at baseline and periodically during therapy catches any problem early.
What are the main alternatives if fluconazole cannot be used?
Itraconazole is the most common oral alternative, offering slightly higher efficacy but a higher risk of drug interactions. For severe or disseminated infection, intravenous amphotericinB (deoxycholate or liposomal) remains the gold‑standard, followed by step‑down oral therapy.
Is there a vaccine against paracoccidioidomycosis?
No licensed vaccine exists yet. Research is ongoing, focusing on recombinant protein candidates that could prime the immune system against Paracoccidioides brasiliensis. Until then, prevention relies on environmental control and early treatment.






Shayne Smith
September 23, 2025 AT 22:24So basically fluconazole is the ‘lazy doctor’s best friend’ for this fungus? Makes sense-no IV, no hospital stay, just pop a pill and hope for the best.
Max Manoles
September 25, 2025 AT 19:36Fluconazole’s oral bioavailability of ~90% is remarkable-especially compared to itraconazole’s erratic absorption. The pharmacokinetic profile makes it ideal for resource-limited settings where adherence and monitoring are challenges. Still, the 80–85% cure rate leaves room for relapse, which is why long-term follow-up is non-negotiable.
Billy Schimmel
September 26, 2025 AT 15:31Yeah, I’ve seen patients on it for a year. They don’t die, but they also don’t exactly thrive. Kinda like a Netflix subscription you never cancel.
Katie O'Connell
September 27, 2025 AT 14:24One must acknowledge the methodological rigor inherent in the referenced clinical data; however, the absence of randomized controlled trials comparing fluconazole to itraconazole in endemic regions remains a significant epistemological lacuna in the current literature.
Clare Fox
September 27, 2025 AT 20:28why do we always treat the fungus like its the bad guy? maybe its just trying to survive in a world that keeps chopping down trees and making farmers breathe dirt. just sayin’.
Akash Takyar
September 28, 2025 AT 23:13Fluconazole is a safe, effective, and cost-efficient option; however, it is imperative that clinicians ensure patient compliance, monitor hepatic enzymes, and consider environmental exposure risks in endemic zones. Prevention is better than cure-always.
Arjun Deva
September 29, 2025 AT 00:35Fluconazole? That’s just Big Pharma’s way of keeping people dependent on pills while the real solution-clean air, clean soil, and less coffee farming-is ignored. They don’t want you cured… they want you dosed.
Inna Borovik
September 29, 2025 AT 12:21Let’s be real-85% cure rate? That’s just 1 in 7 people coming back with a vengeance. And the liver toxicity? Yeah, that’s just ‘mild’ until your ALT hits 800. This isn’t a treatment guide-it’s a risk assessment nightmare wrapped in a PDF.
Jackie Petersen
September 30, 2025 AT 16:27Why are we even using American drugs for a disease that only exists in Latin America? Send the pills to them, not the other way around. We’ve got our own problems.
Annie Gardiner
October 1, 2025 AT 03:56What if the fungus isn’t the problem? What if it’s the human need to control everything? Maybe we should just… let it be? Like, let the fungus live. Maybe it’s the real philosopher here.
Rashmi Gupta
October 2, 2025 AT 13:23Fluconazole works? Fine. But why not use the traditional herbal remedies from the Amazon? We’ve been ignoring indigenous knowledge for centuries. Now we’re surprised when the fungus comes back?
Andrew Frazier
October 4, 2025 AT 10:10Look, if you’re from Latin America and you’re breathing dirt while picking coffee, you deserve what you get. Stop blaming the drug. Blame the dirt. Blame the lack of shoes. This isn’t a medical issue-it’s a cultural one.