Polypharmacy Risk Calculator
Assess Your Risk
This tool calculates your risk of frailty based on the number of medications you take and physical signs of frailty.
Your Risk Assessment
Recommended Actions
Important: Always consult your healthcare provider before making any changes to your medications.
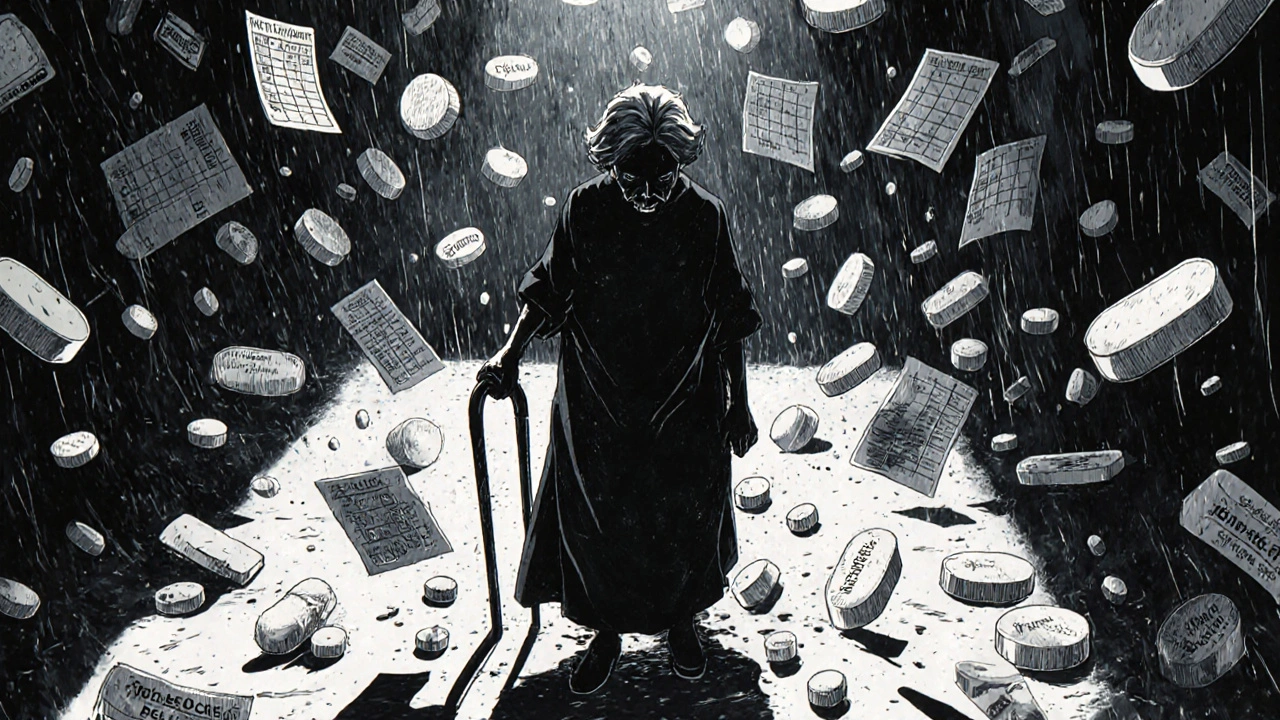
When an older adult is taking five, ten, or even fifteen medications every day, it’s not just about managing disease-it’s about surviving a storm of side effects. Frailty and polypharmacy don’t just coexist; they feed each other. One makes the other worse. And the result? Dizziness that leads to falls, confusion that leads to hospital visits, constipation that leads to more pills, and a life that feels less like living and more like managing a pharmacy.
What Frailty Really Means in Older Adults
Frailty isn’t just being old or weak. It’s a specific medical condition defined by five physical signs: unintentional weight loss, constant tiredness, weak grip strength, slow walking pace, and low physical activity. If someone has three or more of these, they’re classified as frail. Two? They’re prefrail-on the edge. And even one or two of these signs can be a red flag that their body is struggling to cope.What’s alarming is how common this is. In a study of over 3,600 older adults, nearly 9% were frail. But here’s the catch: the more medications they took, the more likely they were to be frail. Each extra pill increased the odds of frailty by 12%. That’s not a coincidence. It’s a pattern.
Frail people don’t process drugs the same way younger people do. Their kidneys and liver slow down. Their bodies hold onto medications longer. A dose that’s safe for a 50-year-old can overwhelm an 80-year-old with frailty. That’s why a blood pressure pill meant to help can end up causing dizziness, falls, or even kidney damage.
Polypharmacy: When More Pills Mean More Problems
Polypharmacy means taking five or more medications daily. Hyper-polypharmacy? Ten or more. These numbers aren’t just statistics-they’re daily realities for millions of older adults.In 1999, about 23% of older U.S. adults were on five or more meds. By 2018, that number jumped to 44%. Among those with heart disease? Over 60%. For people with diabetes? More than half. And it’s not just about chronic illness. Sometimes, one doctor prescribes a drug for a symptom, another prescribes another for the side effect of the first, and a third prescribes something to fix the side effect of the second. It’s a chain reaction.
And the consequences? Hospital stays. Falls. Confusion. Memory loss. Constipation. In one study, 73% of nursing home residents on eight or more medications had constipation. Another 62% reported dizziness. These aren’t side effects you can ignore-they’re safety risks.
The Vicious Cycle: How Frailty and Polypharmacy Trap Each Other
It’s not just that frail people take more pills. It’s that taking more pills makes them frailer.A long-term study followed older adults for eight years. Those taking seven or more medications were 2.5 times more likely to become frail. Why? Because many of these drugs affect the brain, balance, digestion, and energy levels. Anticholinergics-common in antidepressants, bladder meds, and sleep aids-can cause confusion and memory loss. Blood pressure drugs can drop blood pressure too low, leading to fainting. Pain meds can cause constipation, which leads to more laxatives, which leads to electrolyte imbalances.
And it works the other way too. When someone becomes frail, they’re more likely to develop new health problems. A fall leads to a fracture, which leads to pain meds, which leads to constipation, which leads to a laxative, which leads to more pills. Each new condition adds another medication. The cycle tightens.
Research shows that frailty and polypharmacy don’t just add up-they multiply. Together, they cut quality of life in half. People report less energy, less independence, and more fear. And the worst part? Many don’t realize their meds are part of the problem.
Who’s at Highest Risk?
Not everyone faces the same level of risk. Women are more likely to be on multiple medications than men-nearly 49% vs. 39%. Non-Hispanic White older adults have higher rates than Black or Hispanic peers. People with less education are more likely to be on ten or more drugs.But the biggest risk factor? Fragmented care. If you see five different doctors-cardiologist, endocrinologist, neurologist, orthopedist, and primary care-each one may add a medication without knowing what the others prescribed. A study found that 67% of older adults on multiple drugs had care split across specialists with no one looking at the full picture.
Hospitalized patients are the most vulnerable. Over 96% of them are on five or more medications. That’s not because they need them-it’s because the system defaults to adding, not subtracting.
Tools That Work: Beers Criteria, START/STOPP, and Deprescribing
There are tools to help. The Beers Criteria, updated in 2019 by the American Geriatrics Society, lists medications that are risky for older adults-like benzodiazepines for sleep or certain anticholinergics. The START/STOPP criteria go further: they tell doctors not just what to stop, but what to start. For example, if someone has osteoporosis, they should be on calcium and vitamin D-even if they’re on ten other drugs.But tools only work if they’re used. Only 38% of U.S. hospitals have electronic alerts for these guidelines. Most doctors don’t have time to review every med during a 15-minute visit. And patients? Many are terrified to stop anything. They’ve been told these pills are life-saving. What if they die without them?
That’s where deprescribing comes in. It’s not about taking away meds-it’s about removing the ones that do more harm than good. The ‘3-Step Method’ developed by Dr. Cynthia Boyd at Johns Hopkins works like this:
- Review-Go through every pill, one by one. Ask: Is this still needed? What’s it for?
- Discuss-Talk to the patient. What are their goals? Do they want to feel more energy? Walk without help? Avoid hospital visits?
- Monitor-Taper slowly. Watch for changes. Reassess in 2-4 weeks.
In trials, this method reduced inappropriate meds by 28% in six months-with 92% of patients sticking with the plan. And here’s the best part: 76% of people in the EMPOWER trial who stopped one or more unnecessary drugs reported a 32% improvement in quality of life.

Real Solutions: Who’s Making a Difference?
The most effective changes aren’t happening in big hospitals-they’re happening where care is coordinated.Pharmacist-led medication reviews reduce adverse events by 34%. Geriatric clinics that do full assessments-checking mobility, cognition, nutrition, and meds-cut polypharmacy by 22% in a year. Programs like the ‘Medication Check-Up’ teach patients how to ask questions: “Why am I on this?” “What happens if I stop?” “Is there a simpler way?” Those who went through it improved their understanding by 47%.
Technology is catching up too. In January 2024, the FDA approved the first AI-powered tool called MedWise Risk Score. It analyzes all a patient’s meds and predicts which combinations are most likely to cause harm. In testing, it cut adverse events by 37%.
And now, the American Geriatrics Society’s Age-Friendly Health Systems initiative is rolling out the 4Ms Framework across nearly 3,000 U.S. hospitals:
- What Matters-What does the patient care about?
- Medication-Are these drugs helping or hurting?
- Mentation-Is there confusion or depression?
- Mobility-Can they move safely?
Hospitals using this approach have cut inappropriate polypharmacy by 24%.
What You Can Do
If you or a loved one is on five or more medications, here’s what to do next:- Ask for a full medication review-don’t wait for an annual visit. Request it now.
- Bring a list of every pill, vitamin, and supplement-even the ones you skip.
- Ask: “Which of these are absolutely necessary? Which ones could be stopped?”
- Ask about non-drug options: Can physical therapy replace a pain med? Can diet fix constipation instead of laxatives?
- Ask who’s in charge of the whole list. Is there one doctor-or a pharmacist-who’s coordinating everything?
Don’t be afraid to question. You’re not being difficult-you’re being smart. The goal isn’t to take fewer pills. It’s to take the right ones.
Why This Matters More Than Ever
Medication errors in older adults cost the U.S. system $30 billion a year. They cause 125,000 to 300,000 preventable deaths annually. But behind every number is a person-someone who used to walk the dog, cook dinner, or play with grandkids-and now feels too tired, too dizzy, too confused to do any of it.Reducing polypharmacy isn’t about cutting corners. It’s about restoring dignity. It’s about giving someone back their energy, their balance, their peace of mind. And the evidence is clear: when you take away the unnecessary, the right things often get stronger.
Frailty and polypharmacy aren’t inevitable. They’re treatable. And the first step isn’t a new prescription. It’s asking: “Do I really need this?”
How many medications is too many for an older adult?
Five or more daily medications is considered polypharmacy, and it’s linked to higher risks of side effects, falls, and frailty. Ten or more is called hyper-polypharmacy and carries even greater danger. The goal isn’t just to reduce numbers-it’s to make sure every pill is necessary, safe, and aligned with the person’s goals.
Can stopping medications make someone weaker?
Sometimes, yes-but only if done carelessly. Stopping a needed blood pressure or heart medication abruptly can be dangerous. But many older adults are on drugs that were prescribed years ago for a condition that’s no longer active-or for a side effect of another drug. Deprescribing, when done slowly and with monitoring, often improves strength, energy, and balance. Studies show people feel better after stopping unnecessary pills.
Why do doctors keep prescribing more meds instead of stopping?
Most doctors want to help, but they’re under time pressure. A typical visit lasts 15 minutes, and reviewing 10+ meds can take 20-30 minutes. Many don’t have access to a full medication list or tools like Beers Criteria or START/STOPP. Also, patients often fear stopping meds, so doctors avoid the conversation. But that’s changing-geriatric pharmacists and structured reviews are making deprescribing easier and safer.
What’s the difference between Beers Criteria and START/STOPP?
Beers Criteria focuses on medications that are potentially inappropriate for older adults-like certain sleep aids or painkillers. START/STOPP goes further: STOPP identifies bad prescriptions, and START identifies missed opportunities-like not prescribing a bone-strengthening drug to someone with osteoporosis. Together, they give a complete picture: what to stop and what to start.
Are there apps or tools to help manage multiple medications?
Yes. Apps like Medisafe and Round Health help track doses, set reminders, and flag potential interactions. More advanced tools like MedWise Risk Score (FDA-approved in 2024) analyze all medications together and predict which combinations are most likely to cause harm. These aren’t replacements for professional review-but they’re powerful aids for patients and caregivers.
How long does it take to see results after stopping a medication?
It varies. Some side effects, like dizziness or constipation, can improve within days. Others, like cognitive fog from anticholinergics, may take weeks. The key is to stop one med at a time and monitor closely. Most successful deprescribing plans include a follow-up visit or check-in within 2-4 weeks to see how the person is feeling.






Nosipho Mbambo
November 21, 2025 AT 01:27Wow. Just... wow. This is the most overwhelming thing I've read all week. I'm not even old and I'm already scared to take aspirin.
daniel lopez
November 22, 2025 AT 01:22Of course this is happening. Big Pharma has been pushing pills since the 70s. They don't want you healthy-they want you dependent. The FDA? Controlled by lobbyists. The Beers Criteria? Ignored by every hospital that takes Medicare. You think this is about medicine? It's about profit. And they're killing old people with bureaucracy and branded capsules. Wake up. This isn't medical-it's corporate genocide.
Katie Magnus
November 22, 2025 AT 20:52Okay but like... why are we even pretending that old people should be walking around like they're 30? I mean, if you're 85 and your knees are toast, just sit down. Stop trying to ‘be active.’ Let your body rest. And if you need a pill to sleep? Fine. But don't act like you're some hero for ‘deprescribing.’ You're just scared of aging. I'm not. I take 14 pills and I look fabulous. Deal with it.
King Over
November 23, 2025 AT 02:30my grandma took 12 pills a day for 10 years and lived to 94. she never complained. she just ate oatmeal and watched judge judy. maybe the problem isn't the pills. maybe it's the noise.
Johannah Lavin
November 23, 2025 AT 13:33Y'all. I just read this and I'm crying. 😭 My nana was on 11 meds and she stopped walking because she was dizzy all the time. We did a med review with a pharmacist last year and they cut 4 of them. She started dancing again in the kitchen. 🕺💃 She says she feels like herself for the first time in 5 years. I’m telling you-this isn’t just medical advice. It’s magic. 🌟 Please, if you’re reading this and you’re caring for someone older-ask for a review. Don’t wait. They deserve to feel alive.
Ravinder Singh
November 25, 2025 AT 06:53Beautifully written and deeply needed. I'm a geriatric nurse in Delhi and I see this daily. Families think more pills = better care. But I've seen patients wake up after stopping a sedative they'd been on for 8 years. Their eyes-light up. It's not about cutting meds. It's about restoring humanity. The 3-step method? That's the gold standard. And yes, the AI tools like MedWise? Game-changers. But none of it matters if we don't listen to the patient. Their goal isn't to live longer-it's to live better. And we keep forgetting that.
Russ Bergeman
November 25, 2025 AT 17:36Wait, so you’re saying we should just... stop giving people meds? That’s insane. Who’s going to pay for the hospital visits when they fall? Who’s going to cover the cost of the broken hips? This isn’t ‘empowerment’-it’s negligence. And you’re just making it worse. And don’t even get me started on ‘non-drug options.’ Physical therapy? For someone who can’t stand up? Please. You’re not helping-you’re just making people feel guilty for being sick.
Dana Oralkhan
November 27, 2025 AT 11:44I’ve been a caregiver for my mom for 7 years. She’s on 8 meds. I didn’t know any of this. I thought the doctors knew best. But after reading this, I scheduled a med review. We cut 2 that were no longer needed. She sleeps better. She laughs more. I wish I’d known sooner. Thank you for writing this. It’s not just information-it’s a lifeline.
Jeremy Samuel
November 27, 2025 AT 21:44frailty my ass. everyone knows the real problem is the government making old people take pills so they stay quiet and dont vote. also the 4ms thing? sounds like a marketing buzzword. i bet it was written by a consultant who’s never met a real senior. just sayin.