Every time you pick up a prescription, you might see two options: the familiar brand-name pill with the flashy packaging, or a smaller, plain tablet with a different color and shape. Many people wonder - is this generic version just a cheap copy? Is it weaker? Less safe? Or worse, is it fake?
The short answer: no. Generic drugs aren’t copies in the way you might think. They’re not knockoffs. They’re not inferior. They’re scientifically proven to work the same way as the brand-name version - and they’ve been holding up to this standard for decades.
What Exactly Makes a Drug "Generic"?
A generic drug must contain the same active ingredient, in the same strength, and delivered the same way as the brand-name drug. That means if you’re taking 10 mg of lisinopril for high blood pressure, the generic version has exactly 10 mg of lisinopril - not 8 mg, not 9 mg, not 9.8 mg. The FDA requires it to be within 99.2% of the exact amount. That’s not a guess. It’s tested in labs using precise methods.
The only differences you’ll see are in the inactive ingredients - things like fillers, dyes, flavors, or coatings. These don’t affect how the drug works. They’re there for practical reasons: to make the pill easier to swallow, to give it a unique look (so it doesn’t copy the brand’s trademarked appearance), or to help it hold together in the bottle. Think of it like two identical cars - same engine, same transmission, same fuel efficiency - but one has leather seats and the other has cloth. The performance? Identical.
How Do We Know Generics Work the Same?
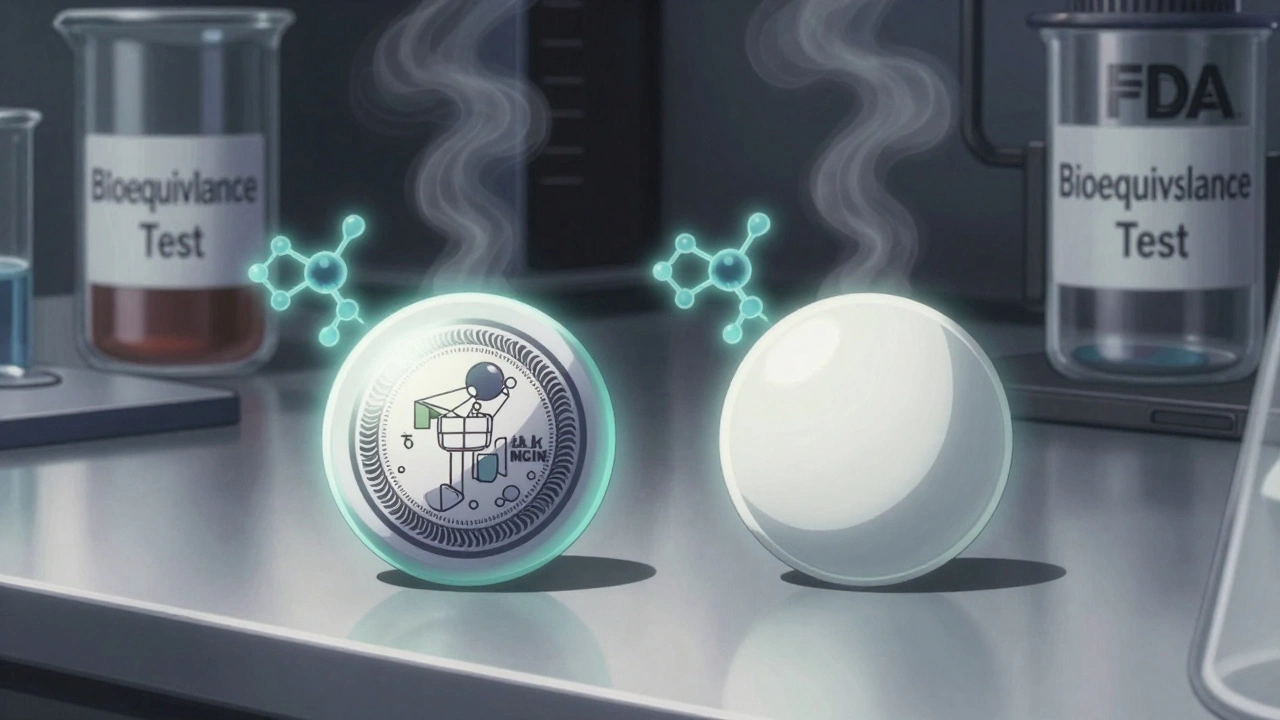
The FDA doesn’t just trust manufacturers. They require every generic drug to pass a strict test called bioequivalence. This means the generic must deliver the same amount of active ingredient into your bloodstream at the same speed as the brand-name drug.
Here’s how it works: volunteers take both the brand and the generic, and their blood is tested over time. Scientists measure two things: how much of the drug gets into the blood (AUC), and how fast it peaks (Cmax). The generic’s results must fall within 80% to 125% of the brand’s. That’s not a wide margin - it’s tight enough to catch even tiny differences. If it doesn’t meet this standard, it’s rejected. No exceptions.
Since 1984, over 14,000 generic drugs have been approved under this system. In 2022 alone, the FDA reviewed more than 2,000 generic applications. Every single one had to prove it matched the original.
Why Are Generics So Much Cheaper?
Brand-name drugs cost a lot because the company had to pay for years of research, clinical trials, and marketing to get approval. That’s why a new drug might cost $500 a month when it first hits the market.
Generic manufacturers don’t have to repeat those expensive studies. Once the patent expires - usually 20 years after the original filing - other companies can apply to make the same drug using the existing safety data. They only need to prove bioequivalence. That cuts development costs by 80-90%.
The result? A 10 mg tablet of atorvastatin (Lipitor) might cost $60 as a brand, but the generic? Around $4. That’s not a gimmick. That’s the power of competition. In the U.S., generics make up 90% of all prescriptions but only 23% of total drug spending. That’s billions saved every year.
Are There Any Exceptions?
Yes - but they’re rare. For most drugs, generics are just as effective. But there’s a small group called narrow therapeutic index (NTI) drugs. These are medications where even a tiny change in blood levels can cause serious problems - either the drug stops working, or it becomes toxic.
Examples include warfarin (a blood thinner), levothyroxine (for thyroid conditions), and some seizure medications like phenytoin. For these, doctors and pharmacists often recommend sticking with one version - brand or generic - and not switching back and forth. It’s not because the generic is unsafe. It’s because small variations, even within FDA limits, could affect someone who’s already finely tuned on the drug.
Still, even here, studies show that 92% of patients on NTI drugs do fine with generics when monitored properly. The FDA has reviewed thousands of cases and found that fewer than 0.3% of reported issues were actually caused by bioequivalence failures.
What Do Real People Say?
On Drugs.com, over 1.2 million reviews show that 82% of people report no difference between generic and brand-name drugs. On Reddit’s pharmacy forums, 67% of users say they’ve never noticed a change after switching. One user wrote: "I’ve been on generic metformin for five years. My A1C is the same. No side effects. Saved me $80 a month. Why would I go back?"
But some people do report minor differences - usually things like stomach upset or a weird taste. These are almost always linked to the inactive ingredients. A person with a sensitivity to a certain dye or preservative might react to one brand but not another. That’s why pharmacists ask if you’ve had reactions to pills before.
A 2022 Kaiser Family Foundation survey found that 78% of insured adults get generics as their first option - and 89% of them are happy with the results. Medicare Part D users saved an average of over $500 a year just by using generics.

Why Do People Still Doubt Generics?
One reason? Misinformation. A Brown University study found that 43% of patients believe generics contain only 20-80% of the active ingredient. That’s completely false. FDA testing shows generics contain nearly the full amount - 99.2% on average.
Another reason? Marketing. Brand-name companies spend millions reminding you of their name. Generic manufacturers don’t advertise. So when you see a plain white pill, your brain might think, "This looks cheap. It must be less effective." But looks don’t determine potency.
Pharmacists spend an average of 3.2 minutes per prescription explaining this. That’s time they could be helping with other questions - if only more people understood the science behind it.
What’s Changing Now?
The generic drug system is getting faster. The FDA’s GDUFA IV plan aims to cut approval times from 38 months to just 10 months by 2027. Why? Because there’s a backlog of complex generics - like inhalers, eye drops, and topical creams - that are harder to copy. These are the next frontier.
Also, biosimilars (the generic version of biologic drugs like Humira or Enbrel) are starting to enter the market. These aren’t simple pills - they’re made from living cells. But they follow the same rule: they must match the original in safety and effectiveness. The first wave of biosimilars is already cutting prices by 30-50%.
And in 2022, Congress passed a law requiring Medicare Part D to automatically switch patients to generics unless the doctor says otherwise. That’s expected to save $156 billion over ten years.
What Should You Do?
If your doctor prescribes a brand-name drug, ask: "Is there a generic?" Most of the time, the answer is yes - and it’s just as good.
If you’re switching from brand to generic, monitor how you feel for the first few weeks. Most people notice nothing. If you do feel different - especially if you’re on a drug like warfarin or levothyroxine - tell your doctor or pharmacist right away. Don’t assume it’s the drug. It might be something else.
And if you’re worried about cost, ask about price. Sometimes, the generic is cheaper. Sometimes, the brand is on sale. But in 95% of cases, the generic is the smarter choice - for your wallet and your health.
Generics aren’t copies. They’re alternatives - proven, tested, and regulated. And for millions of people, they’re the reason they can afford to stay healthy.
Are generic drugs just as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence - meaning they deliver the same amount of medicine into your bloodstream at the same rate. For over 90% of drugs, generics work exactly the same way.
Why do generic drugs look different from brand-name drugs?
U.S. trademark laws require generic drugs to look different from the brand-name version. That means different colors, shapes, or markings. But these changes are only in the inactive ingredients - like dyes or fillers - which don’t affect how the drug works. The active ingredient is identical.
Can generic drugs cause more side effects?
Rarely. Most side effects come from the active ingredient, which is the same in both versions. But some people may react to inactive ingredients like dyes or preservatives. If you notice new side effects after switching, talk to your pharmacist. They can check if the filler or coating changed - and help you switch to another generic version if needed.
Are there any drugs where I should avoid generics?
For most drugs, no. But for narrow therapeutic index (NTI) drugs - like warfarin, levothyroxine, and some seizure medications - small changes in blood levels can matter. Your doctor may recommend sticking with one version (brand or generic) to avoid fluctuations. But even then, many patients use generics safely with proper monitoring.
Do pharmacists automatically substitute generics?
In 49 U.S. states, pharmacists can substitute a generic unless the doctor writes "dispense as written" or the patient requests the brand. You always have the right to ask for the brand-name drug - but you may pay more. In many cases, the generic costs less even if you don’t have insurance.
How long does it take for a generic to become available?
Generics can’t be sold until the brand-name drug’s patent expires - usually 20 years after the patent is filed. But legal challenges, exclusivity periods, or complex manufacturing can delay entry. Some generics appear within months of patent expiry; others take years, especially for complex drugs like inhalers or injectables.
Is it true that generics have less active ingredient?
No. FDA testing shows that generic drugs contain 99.2% of the active ingredient on average - the same as the brand-name version. Claims that generics contain only 20-80% are false and not supported by any scientific evidence.
Why do some people say generics don’t work for them?
Sometimes, it’s not the drug - it’s the switch. If someone has been on a brand-name drug for years and suddenly changes to a generic, they might notice a change in how the pill feels or tastes. That can trigger a nocebo effect - where expecting a problem causes real symptoms. In rare cases, it’s due to an allergy to an inactive ingredient. But studies show 82% of users report no difference in effectiveness.







John Fred
December 12, 2025 AT 14:36Bro, generics are the unsung heroes of modern medicine 🚀. Same active ingredient, same bioequivalence, same results - just without the brand markup. I’ve been on generic metformin for 6 years. My A1C? Rock solid. My wallet? Thank you, FDA. 💪💊
Harriet Wollaston
December 13, 2025 AT 18:50I used to be skeptical too, until my grandma switched to generic levothyroxine and didn’t miss a beat. She said the pill just looked different - same size, same taste, same energy. Sometimes the science just needs a human story to stick. ❤️
Lauren Scrima
December 14, 2025 AT 07:56Ohhh, so the FDA says it’s ‘within 80–125%’? 😏 So… technically, a generic could be 25% weaker? And you’re okay with that? I mean, I guess if you’re okay with your blood pressure meds being a lottery ticket… 🤷♀️
Tommy Watson
December 15, 2025 AT 07:22bro i swear the generic adderall i took last year made me feel like a zombie with a headache and i had to go back to brand because my brain was like ‘who are you and why are you talking to me like this’ 🤯
Richard Ayres
December 15, 2025 AT 12:00It’s worth noting that the 80–125% bioequivalence range is statistically rigorous and validated across thousands of trials. The FDA’s standard is designed to ensure therapeutic equivalence, not just chemical similarity. The variation is not arbitrary - it’s calibrated to clinical outcomes. Most patients experience no difference, and those who do often have underlying sensitivities to excipients, not the active ingredient.
Michael Gardner
December 16, 2025 AT 06:08Yeah sure, ‘scientifically proven’ - until you’re the one who had to switch to generic warfarin and ended up in the ER because your INR went nuts. The system works… for most people. But when it doesn’t, it’s your life on the line. So no, I’m not just gonna trust a label.
Willie Onst
December 18, 2025 AT 03:46You know what’s wild? People think a pill has to look fancy to work. But that’s like saying a Toyota Camry is less reliable than a BMW just because it doesn’t have leather seats. The engine’s the same. The road doesn’t care what color the car is. 🌍
Jennifer Taylor
December 19, 2025 AT 23:09EVERYONE KNOWS BIG PHARMA MAKES THE GENERIC VERSIONS TOO. THEY OWN THE BRAND AND THE GENERIC. THEY’RE JUST PLAYING YOU. THEY WANT YOU TO THINK YOU’RE SAVING MONEY BUT YOU’RE JUST BUYING THE SAME DRUG UNDER A DIFFERENT NAME. THE FDA IS IN ON IT. 🕵️♀️💊
nithin Kuntumadugu
December 20, 2025 AT 23:09u think u r smart with ur FDA stats but in india we know generics r just chinese powder in capsules with no quality control. u think ur safe but ur body is just a lab rat for big pharma. 😒
sharon soila
December 22, 2025 AT 08:50Let me be clear: the FDA’s bioequivalence standards are among the most stringent in the world. Generics are not ‘copies.’ They are equivalent. And for those who cannot afford brand-name medication, they are a lifeline. Choosing a generic is not a compromise. It is a responsible, informed, and compassionate decision.
nina nakamura
December 24, 2025 AT 01:58People who say generics are fine are either lying or naive. If it worked the same, why do drug companies spend billions on branding? Why do pharmacies push generics? Because they make more money. The system is rigged. End of story.