Millions of people with asthma and COPD rely on inhalers to breathe easier. But here’s the hard truth: most of them are using them wrong. Studies show 70 to 90% of patients don’t get the full benefit because their technique is off. That means up to 90% of the medicine is wasted-stuck in your mouth, throat, or coughed right back out. You’re not just losing effectiveness-you’re risking flare-ups, ER visits, and long-term lung damage. The device doesn’t matter if you don’t know how to use it.
Why Technique Matters More Than the Device
You might think the brand or type of inhaler makes the biggest difference. It doesn’t. What matters most is whether you’re actually getting the medicine into your lungs. A 2022 study in Respiratory Medicine found only 23% of people could press the inhaler and breathe in at the same time without training. That’s not a failure of willpower-it’s a failure of instruction. Most people are handed an inhaler, told to ‘use as needed,’ and left to figure it out.
Here’s the reality: even the best inhaler is useless if you don’t time your breath right. The difference between correct and incorrect use? Your lungs get 8-30% of the dose with bad technique. With proper technique? 40-60%. That’s a 100% increase in medication reaching where it’s supposed to go. The American Lung Association says technique is the single most important factor in effectiveness-more than the device itself.
The Three Main Types of Inhalers (and How They Work)
Not all inhalers are the same. There are three main types, and each requires a completely different approach.
- Metered-Dose Inhalers (MDIs) - These are the classic canisters with a mouthpiece. They spray medicine using a propellant. You press down and breathe in at the same time. Sounds simple? It’s not. Most people press too early, too late, or too hard. The medicine hits your tongue and throat instead of your lungs.
- Dry Powder Inhalers (DPIs) - These don’t use spray. Instead, you breathe in fast and hard to pull the powder into your lungs. Think of it like snorting a tiny amount of medicine. If you don’t inhale with enough force-60-90 liters per minute-you won’t get the full dose. That’s why they’re often a bad fit for older adults or people with severe COPD who can’t generate strong breaths.
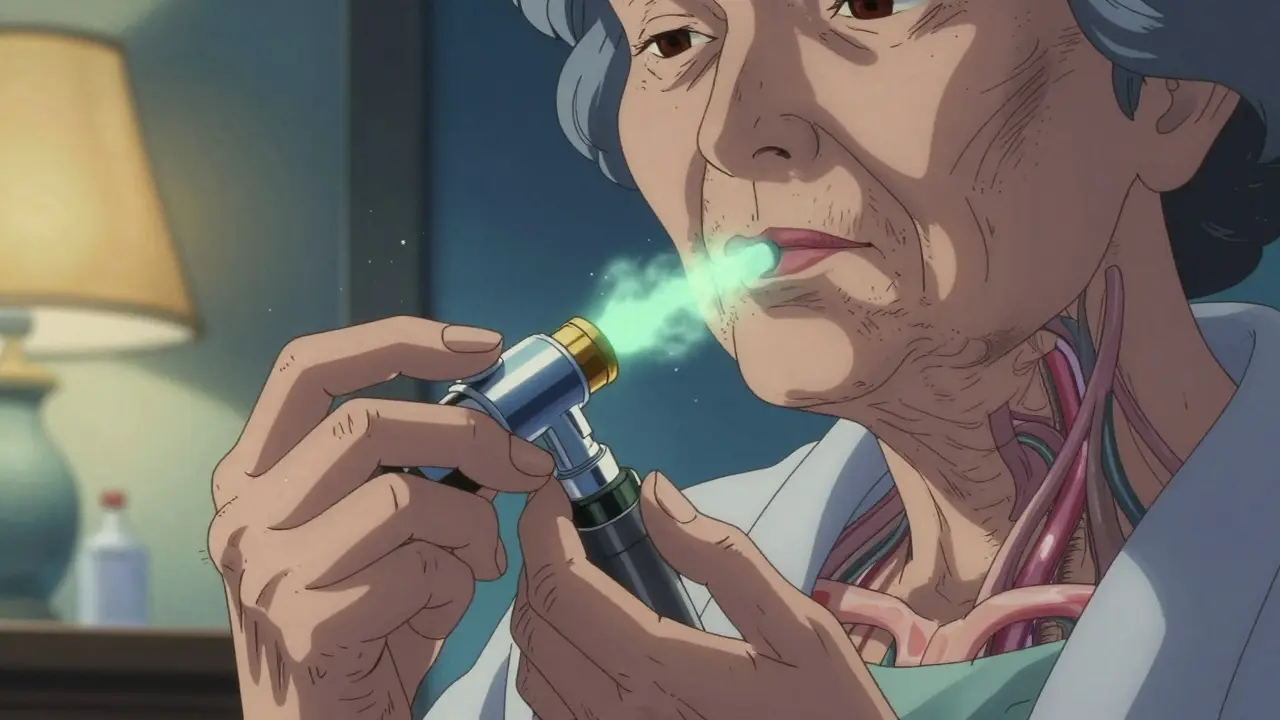
- Soft Mist Inhalers - These are newer. They release a slow, fine mist over 1.5 seconds. You don’t need perfect timing, but you still need to breathe in deeply and hold. They’re easier for people who struggle with coordination, but they’re also more expensive and less common.
The key takeaway? You can’t treat them all the same. Using a DPI like an MDI? You’ll get almost nothing. Using an MDI without a spacer? You’re wasting most of your dose.
How to Use an MDI the Right Way (Step by Step)
If you’re using a metered-dose inhaler, here’s what you need to do-every single time:
- Remove the cap and shake the inhaler well for 5 seconds.
- Stand or sit up straight. Tilt your head back slightly.
- Breathe out fully-away from the inhaler.
- Place the mouthpiece in your mouth and seal your lips tightly around it.
- Press the canister to release the medicine at the very start of a slow, deep breath (like sipping a thick milkshake through a straw).
- Keep breathing in slowly for 3-5 seconds until your lungs feel full.
- Hold your breath for 10 seconds. This lets the medicine settle in your airways.
- Breathe out slowly through your nose.
And here’s the part most people skip: wait 60 seconds between puffs. If you need a second puff, don’t rush. Wait a full minute. Also, if your inhaler contains steroids (like fluticasone or budesonide), rinse your mouth with water afterward. It cuts your risk of oral thrush by 75%.
Why Spacers Are a Game-Changer (But Only for MDIs)
A spacer is a plastic tube that attaches to your MDI. It holds the medicine after you press the canister, so you don’t have to time your breath perfectly. You press, then breathe in slowly from the spacer. It’s like having a mini reservoir that gives you extra time.
The numbers don’t lie: using a spacer with an MDI increases lung delivery by 70-100%. That’s the same as doubling your dose-without taking more medicine. The Global Initiative for Asthma (GINA) recommends spacers for everyone, especially children, older adults, and anyone who struggles with coordination.
But here’s the trap: never use a spacer with a dry powder inhaler. It will trap the powder and block it from reaching your lungs. A 2022 study in the Journal of Aerosol Medicine showed a 50-70% drop in effectiveness when spacers were used with DPIs. Know your device. Mixing them up wastes medicine and puts your health at risk.
What About Dry Powder Inhalers?
DPIs like the Diskus, Ellipta, or Turbuhaler don’t need timing-they need force. Here’s how to use them:
- Load the dose as instructed (some require twisting, others slide a lever).
- Hold the device upright. Never tilt it sideways.
- Breathe out fully-away from the device.
- Place your lips tightly around the mouthpiece.
- Inhale quickly and deeply-like you’re trying to suck a straw dry in one hard pull.
- Hold your breath for 10 seconds.
- Breathe out slowly.
Important: never open the capsule or try to shake the powder out. That’s a common mistake. The device is designed to release the powder only when you inhale with enough force. If you hear a click but don’t feel the powder, you didn’t inhale hard enough. Try again.
People over 65 often struggle with DPIs because their lung strength has dropped. If you’re older or have advanced COPD, your doctor might recommend switching to an MDI with a spacer instead.
Common Mistakes (And How to Fix Them)
Based on thousands of patient reports and clinical studies, here are the top mistakes-and how to avoid them:
- Not shaking the inhaler - 45% of users skip this. Shake it for 5 seconds before every puff. If you don’t, the medicine settles and you get uneven doses.
- Exhaling into the device - 27% of people breathe out into the mouthpiece before inhaling. That’s like blowing air into a balloon before filling it. You’re pushing the medicine out before it even gets in. Always exhale away from the inhaler.
- Not holding your breath - 63% of users don’t hold their breath for 10 seconds. Holding it lets the medicine stick to your airways. If you exhale right away, you lose most of it.
- Using multiple inhalers without training - The European Respiratory Society says mixing devices without proper instruction cuts effectiveness by 35-50%. If you have two inhalers, learn one at a time.
- Storing inhalers in hot places - Leaving your inhaler on a sunny windowsill or in your car can drop its effectiveness by 15-20%. Keep it at room temperature (20-25°C).

When to Ask for Help
Most people don’t realize they’re using their inhaler wrong until they’re in the ER. If you’ve had a flare-up in the last 6 months, or if your inhaler doesn’t seem to be working like it used to, it’s time to get checked.
The UK Inhaler Group and the American Lung Association both recommend that your doctor or nurse demonstrate your technique at every visit. If they don’t offer, ask. Say: “Can you watch me use my inhaler and tell me if I’m doing it right?” That’s your right as a patient.
There are also free video tutorials from the American Lung Association and Asthma UK. Watch them with your inhaler in hand. Pause and repeat. Do it in front of a mirror. See if your lips are sealed. Watch your head position. Notice if you’re puffing too fast or too slow.
What’s Changing in 2026?
The future of inhalers is getting smarter. The FDA approved smart inhalers in 2021-devices with sensors that track when and how you use them. These can tell if you’re inhaling too slowly, not holding your breath, or missing doses. One study showed they improve technique accuracy by 92%.
By 2025, 40% of new inhalers are expected to include digital tracking. Some are even being designed to automatically release medicine when you breathe in just right-no timing needed. But until those become standard, the old-school technique still matters most.
Right now, your best tool isn’t a fancy device. It’s awareness. It’s practice. It’s asking for help when you’re unsure. Because breathing shouldn’t be a guessing game.
How do I know if I’m using my inhaler correctly?
The easiest way is to ask your doctor or pharmacist to watch you use it. Many clinics have mirrors or training devices to help. You can also record yourself using your inhaler and compare it to official videos from the American Lung Association or Asthma UK. If you’re still having symptoms despite using your inhaler regularly, poor technique is likely the cause.
Can I use my inhaler without a spacer?
You can, but you won’t get the full benefit. Without a spacer, only 8-30% of the medicine reaches your lungs. With a spacer, that jumps to 40-60%. Spacers are especially important for children, older adults, and anyone with trouble coordinating their breath. They’re not optional-they’re essential for MDIs.
Why does my inhaler sometimes taste bitter?
That’s medicine stuck in your mouth or throat-not your lungs. It happens when you don’t breathe in slowly enough or don’t hold your breath. Rinsing your mouth after using steroid inhalers helps reduce this and prevents oral thrush. If the taste is strong and frequent, your technique likely needs adjustment.
Are dry powder inhalers better than metered-dose inhalers?
Neither is better overall. DPIs deliver more medicine to the lungs when used correctly, but they require strong, fast inhalation. MDIs with spacers are just as effective and easier for people who can’t generate enough breath force-like older adults or those with severe COPD. The best device is the one you can use correctly every time.
What should I do if I miss a dose?
If you miss a dose of your maintenance inhaler (like a steroid), take it as soon as you remember. If it’s almost time for your next dose, skip the missed one. Never double up. For rescue inhalers (like albuterol), use them only when you’re having trouble breathing. Don’t use them to make up for a missed daily dose.
How often should I clean my inhaler?
Clean your MDI mouthpiece at least once a week. Remove the metal canister, rinse the plastic cap and mouthpiece with warm water, and let it air-dry overnight. Don’t wash the metal part or put it in the dishwasher. DPIs don’t need cleaning-just keep them dry and don’t open the capsule. Moisture can ruin the powder.
Next Steps: Take Control of Your Breathing
Start today. Grab your inhaler. Watch a 2-minute video from the American Lung Association. Do it in front of a mirror. Practice the steps. Then, ask your doctor to check your technique at your next visit. Don’t wait until you’re gasping for air. Proper inhaler use isn’t a one-time lesson-it’s a daily habit. And it’s the single most effective thing you can do to stay out of the hospital and breathe easier.