Medication Side Effect Risk Checker
This tool helps you determine if your symptoms could indicate a dangerous medication reaction. Based on FDA guidelines and medical research, it identifies symptoms that require immediate medical attention versus those that may be less serious.
Important: This is not a substitute for professional medical advice. If you're experiencing life-threatening symptoms, call 911 immediately.
Select Your Symptoms
Urgent Results
Most people take medication without a second thought. But what if the very thing meant to help you could quietly turn dangerous? You might feel a little dizzy after your blood pressure pill, or get a dry mouth from your antidepressant. Those are common. But some side effects aren’t just annoying-they’re life-threatening, and they can show up fast. The difference between a mild reaction and a medical emergency often comes down to recognizing the early warning signs before it’s too late.
What Makes a Side Effect Dangerous?
Not all side effects are created equal. A stuffy nose or mild nausea? That’s typical. But when a drug triggers a reaction that harms your organs, disrupts your heart rhythm, or shuts down your breathing, it’s no longer just a side effect-it’s a medical emergency. According to the FDA, over 1.3 million emergency room visits each year in the U.S. are caused by adverse drug reactions. Around 128,000 of those end in death. Many of these cases could have been prevented if the warning signs had been caught early. Dangerous reactions don’t always happen right away. Some show up hours after you take the pill. Others creep in over days or weeks. But the ones that kill? They usually escalate fast. If you start feeling worse within an hour of taking a new medication, don’t wait. Don’t hope it’ll pass. Act.Red Flags That Require Immediate Action
Here’s what you need to watch for-right now, the moment you notice it:- Difficulty breathing or tightness in your throat. This isn’t just a cold. It’s your airway closing. Combine this with swelling in your face, lips, or tongue, and you’re likely having anaphylaxis-a severe allergic reaction that can kill in minutes.
- Hives, rash, or skin peeling. A mild itch might be nothing. But if the rash spreads quickly, blisters, or comes with fever and swelling, it could be DRESS syndrome or Stevens-Johnson syndrome. Both are rare but deadly.
- Chest pain or irregular heartbeat. If your heart feels like it’s racing (over 100 beats per minute), fluttering, or skipping, especially with dizziness or fainting, stop what you’re doing. This could signal a dangerous arrhythmia. Untreated, it can lead to cardiac arrest.
- Unusual bleeding or bruising. You didn’t bump into anything, but you’re covered in bruises? Or your gums bleed when you brush? This could mean your blood isn’t clotting properly-a side effect of blood thinners, NSAIDs, or even some antibiotics.
- Severe vomiting or blood in stool. It’s one thing to feel queasy. It’s another to vomit for hours or see dark, tarry stools. This could point to internal bleeding or pancreatitis, especially if you’re taking weight-loss drugs like semaglutide or tirzepatide.
- Yellow skin or eyes. Jaundice isn’t just a sign of liver problems-it’s a red flag for drug-induced liver injury. When paired with severe stomach pain, it’s an emergency. Left untreated, liver failure can happen in under 48 hours.
- Seizures or loss of consciousness. Even if you’ve never had a seizure before, a new one after starting a medication is a clear signal that your brain is reacting dangerously.
- Extreme drowsiness or confusion. If you’re nodding off beyond what the label says, or can’t wake up easily, it could be central nervous system depression. This is especially risky with opioids, benzodiazepines, or sleep aids.
These symptoms don’t always appear together. But if you notice even one of them-especially within hours of taking a new drug-call 911 or go to the nearest emergency room. Don’t text your doctor. Don’t wait until morning. Time is everything.
Signs That Are Slower But Just as Dangerous
Some life-threatening reactions don’t scream for help. They whisper. And that’s when people get hurt.- Decreased urine output. If you’re not peeing as much as usual, or your urine looks dark, your kidneys might be failing. This can happen with NSAIDs, certain antibiotics, or contrast dyes used in imaging tests.
- Swelling in your legs or belly. Fluid retention isn’t just weight gain. It can mean your heart or liver is struggling. When paired with fatigue and shortness of breath, it’s a red flag for organ damage.
- Unexplained fatigue or weakness. You’re not sleeping more, but you’re exhausted all the time? This could signal drug-induced anemia, where your body stops making enough red blood cells.
- Fever with swollen lymph nodes. If you’ve been on a new medication for a week or two and suddenly feel flu-like with swollen glands, it could be serum sickness-a delayed immune reaction that can damage kidneys and joints.
- Confusion or memory loss. Especially in older adults, this isn’t just aging. It could be drug toxicity. Many medications build up in the body as we age, and even small doses can become toxic.
These signs might seem vague. But if they’re new, persistent, and appear after starting a medication, they’re not normal. Talk to your doctor within 24 hours. Don’t brush them off.
Who’s at Highest Risk?
Some people are more likely to have dangerous reactions. If you fit any of these categories, be extra vigilant:- People over 65. Your body processes drugs slower. You’re 2.7 times more likely to have a bad reaction than someone younger.
- Those taking five or more medications. This is called polypharmacy. The more drugs you take, the higher the chance they’ll interact in harmful ways. One in two older adults are in this group.
- People with kidney or liver disease. These organs clear drugs from your body. If they’re not working well, medications can build up to toxic levels.
- Those with known allergies. If you’ve had a reaction to a drug before, you’re at higher risk for another-even if it’s a different brand or form.
And here’s something most people don’t realize: look-alike, sound-alike drugs cause 12% of dangerous errors. Insulin and heparin are two of the most commonly confused. One wrong dose can kill.
What to Do When You Suspect a Dangerous Reaction
Step 1: Stop taking the medication-but only if your doctor told you to. Never quit cold turkey. Stopping beta-blockers or antidepressants suddenly can cause heart attacks or seizures. Step 2: Call 911 if you have any of the life-threatening signs listed above. Don’t drive yourself. Don’t wait. Emergency responders have epinephrine and can stabilize you on the way. Step 3: For less urgent but still serious symptoms-like unusual bleeding, severe nausea, or jaundice-call your doctor or pharmacist within 24 hours. Keep a list of all your meds, including supplements and over-the-counter drugs. Bring them in a brown bag to your appointment. This is called the Brown Bag Method, and it helps your provider spot dangerous interactions. Step 4: Report the reaction. Go to the FDA’s MedWatch website or ask your doctor to file a report. These reports help identify dangerous drugs before more people get hurt.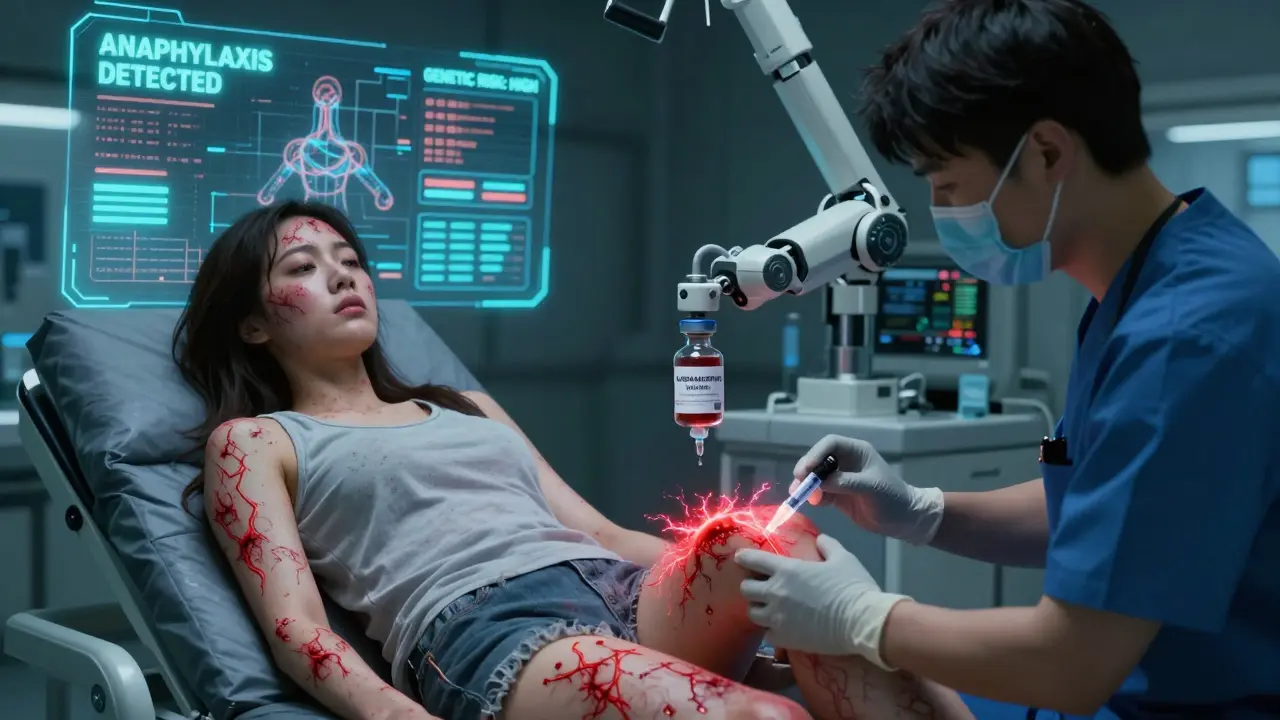
How Technology Is Helping Prevent These Reactions
The good news? Tools are getting smarter. Mayo Clinic’s new AI dashboard analyzes your age, weight, kidney function, and current meds to predict your risk of a bad reaction with 89% accuracy. The NIH’s Pharmacogenomics Research Network tests your genes before prescribing certain drugs-like carbamazepine-to see if you’re genetically prone to severe side effects. Early results show a 47% drop in dangerous reactions. By 2026, smart packaging for high-risk drugs will send alerts if you take too much or too little. Wearables like Apple Watches will soon detect medication-induced heart rhythm problems automatically. These aren’t sci-fi-they’re coming fast.Bottom Line: Trust Your Body, Not Just the Label
Medications save lives. But they can also hurt you-if you ignore the signs. Common side effects are usually harmless. Dangerous ones are not. They come fast. They come quiet. They don’t always look like what you expect. Your body gives you clues. Listen to them. If something feels wrong after starting a new drug, don’t second-guess yourself. Call your doctor. Call 911. Save your life before it’s too late.Can medication side effects show up weeks after starting a drug?
Yes. While some reactions happen within minutes or hours-like anaphylaxis-others can take days or weeks to appear. Rashes, fever, joint pain, fatigue, and liver or kidney problems often develop slowly. This is why it’s important to monitor your body even after you’ve been on a medication for a while. If you notice new symptoms, especially after a change in dosage or adding a new drug, tell your doctor right away.
Is it safe to stop a medication if I think it’s causing side effects?
No-not without talking to your doctor first. Stopping certain drugs suddenly can be dangerous. For example, quitting beta-blockers, antidepressants, or anti-seizure meds abruptly can trigger heart attacks, seizures, or severe withdrawal symptoms. Even if you think the side effect is bad, don’t quit cold turkey. Call your provider. They can help you taper off safely or switch to a different drug.
How do I know if my symptoms are from a drug or just a cold or flu?
Timing matters. If your symptoms started within hours or days after taking a new medication-or changed after a dosage increase-it’s likely related. A cold usually comes with a sore throat, runny nose, and mild fever that builds over a few days. A drug reaction often hits harder and faster: sudden swelling, rash, trouble breathing, or chest pain. When in doubt, assume it’s the medication until proven otherwise. It’s better to be safe than sorry.
Are older adults more at risk for dangerous medication side effects?
Yes. As we age, our liver and kidneys process drugs more slowly, so medications stay in the body longer and can build up to toxic levels. About 44% of adults over 65 take five or more medications, which increases the risk of dangerous interactions. The American Geriatrics Society says older adults are 2.7 times more likely to have serious side effects than younger people. Regular medication reviews and using the Brown Bag Method can help reduce this risk.
Can over-the-counter drugs cause dangerous side effects?
Absolutely. Many people assume OTC meds are harmless, but that’s not true. NSAIDs like ibuprofen or naproxen can cause internal bleeding, kidney damage, or heart problems. Acetaminophen (Tylenol) in high doses can lead to liver failure. Even antihistamines and sleep aids can cause confusion, falls, or dangerous interactions with prescription drugs. Always tell your doctor what OTC meds and supplements you’re taking.
What should I do if I think I’m having a reaction but I’m not sure it’s serious?
When in doubt, err on the side of caution. Call your pharmacist or doctor. They can help you decide if it’s something you can monitor at home or if you need to go to the ER. Keep a symptom journal: write down what you took, when you took it, and what happened. This helps your provider spot patterns. Don’t downplay symptoms just because they seem mild. Early action can prevent a small problem from becoming a life-threatening one.
How can I reduce my risk of dangerous side effects?
Keep a complete list of all your medications-including vitamins, supplements, and OTC drugs-and review it with your doctor or pharmacist every 3 to 6 months. Ask: "Is this still necessary?" and "Could this interact with anything else I’m taking?" Avoid taking more than five drugs if possible. Use one pharmacy so your pharmacist can track interactions. And never ignore new symptoms-especially if they start after a medication change.




Tony Du bled
December 22, 2025 AT 07:20Been on blood pressure meds for 7 years. Started getting this weird rash last month. Thought it was laundry detergent. Turned out to be DRESS syndrome. ER saved my life. Don’t ignore skin changes. Even if it’s just a little itchy.
Kathryn Weymouth
December 23, 2025 AT 09:41The distinction between common side effects and life-threatening reactions is critical, and this post articulates it with remarkable clarity. I particularly appreciate the emphasis on timing-symptoms emerging hours or days post-administration are often misattributed to viral illnesses, delaying intervention. The inclusion of pharmacogenomics and AI risk prediction tools reflects a necessary evolution in clinical safety protocols.
Julie Chavassieux
December 23, 2025 AT 11:34My aunt died from a drug reaction. No one saw it coming. They said she was just tired. Just a little confused. Just a little bruised. Just a little off. Until she wasn’t.
Herman Rousseau
December 24, 2025 AT 23:51This is the kind of post that needs to go viral. Seriously. I work in pharmacy and I see people ignoring red flags every single day. If you’re on 5+ meds, get a brown bag review. If you feel weird after a new pill-call your doc TODAY. Don’t wait. Don’t Google it. Don’t hope it goes away. Your life isn’t a gamble.
Vikrant Sura
December 25, 2025 AT 15:52Why are we even talking about this? Just don’t take drugs if you’re scared. Simple.
Candy Cotton
December 26, 2025 AT 04:11As an American citizen, I find it unacceptable that our healthcare system requires citizens to self-diagnose life-threatening drug reactions. This is not a matter of personal responsibility-it is a systemic failure of regulation, oversight, and pharmaceutical accountability. We must demand federal action, not rely on Brown Bag Methods.
Jeremy Hendriks
December 27, 2025 AT 09:01Medication is the modern sacrament-blind faith in the white pill, the silent ritual of swallowing destiny. But what if the gods of chemistry are fickle? What if the body, that ancient machine, remembers every toxin, every imbalance, every whispered betrayal of biology? We don’t take pills-we surrender to algorithms written by corporations with no soul. And yet we call it progress.
Gabriella da Silva Mendes
December 28, 2025 AT 23:03OMG I just realized I’ve been taking ibuprofen every day for 3 years 😭 I thought it was just ‘normal’ to have a headache. Now I’m scared I’ve ruined my kidneys. I’m going to the pharmacy tomorrow with my brown bag. Also I just found out my grandma died from a drug reaction and no one told me. I’m crying. 💔
Kiranjit Kaur
December 30, 2025 AT 17:46This is so important. I’m from India and we don’t talk about this enough. People here buy antibiotics over the counter like candy. My cousin took 3 different painkillers at once and ended up in ICU. Please share this with your family. Especially older ones. A simple conversation could save a life. 🙏