If you’ve ever felt stuck in a loop of negative thoughts - like "I’m not good enough" or "Nothing ever goes right" - and those thoughts are keeping you from sleeping, working, or even leaving the house, you’re not alone. Millions of people struggle with this. And there’s a well-researched, practical solution that’s been helping people for over 60 years: cognitive behavioral therapy, or CBT.
Unlike talk therapies that dig deep into childhood or past trauma, CBT is focused on today. It asks: What are you thinking right now? What are you doing about it? And how can you change it? The goal isn’t to feel better instantly. It’s to learn skills you can use for life.
How CBT Works: Your Thoughts Shape Your Life
CBT is built on a simple but powerful idea: your thoughts affect your feelings, which affect your behavior. It’s not the situation itself that hurts you - it’s how you interpret it.
Imagine you’re at work and your boss doesn’t say hello. One person thinks, "They’re mad at me. I must have messed up." They feel anxious, avoid their boss, and start overworking to prove themselves. Another person thinks, "They’re probably just stressed. I’ll check in later." They feel calm, keep working, and even offer help.
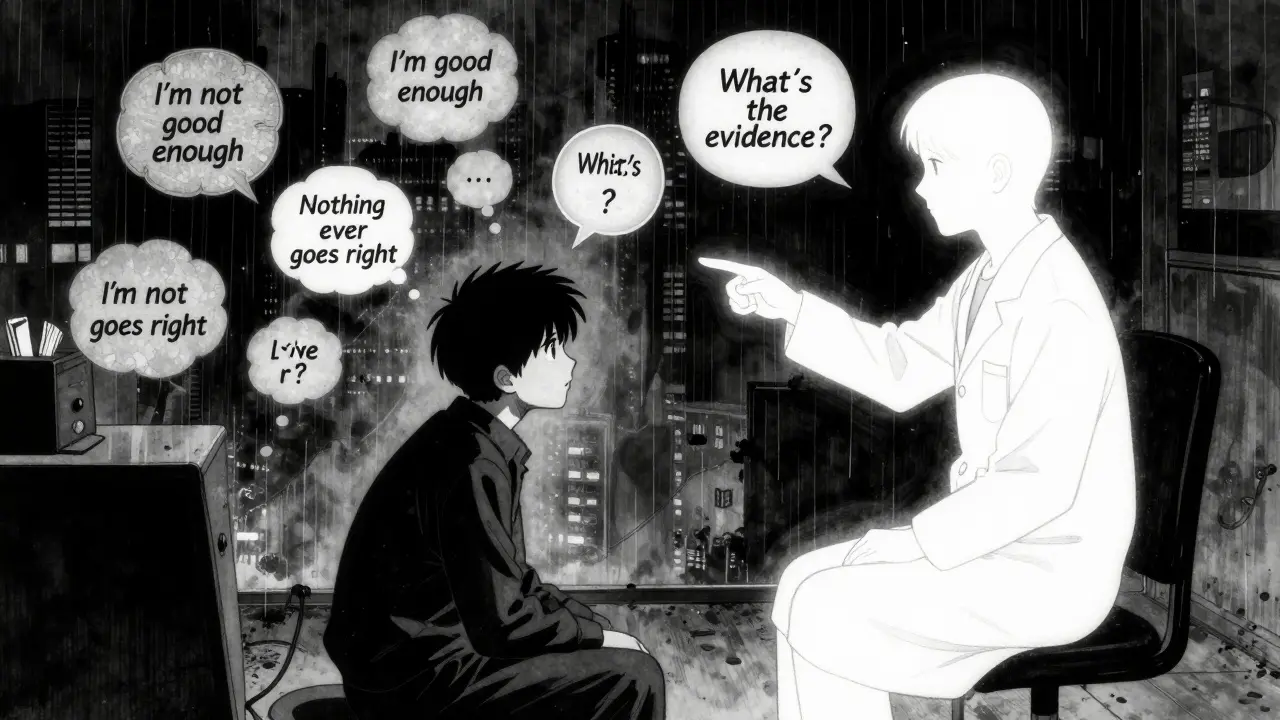
CBT helps you spot the first kind of thinking - the automatic, distorted thoughts that fuel anxiety, depression, or anger. These aren’t just "negative" thoughts. They’re often inaccurate. CBT teaches you to question them.
Psychiatrist Aaron T. Beck first noticed this in the 1960s. He saw that people with depression didn’t just feel sad - they had a pattern of thinking: "I’m worthless," "The world is against me," "The future is hopeless." He called this the cognitive triad. And he proved that changing these thoughts could change how people felt.
The Eight Core Tools of CBT
CBT isn’t one technique. It’s a toolkit. Therapists use eight main strategies, all backed by decades of research:
- Identifying cognitive distortions - like "catastrophizing" ("If I fail this test, my life is over") or "mind reading" ("They think I’m weird").
- Challenging automatic negative thoughts - asking, "What’s the evidence for this? What’s another way to see it?"
- Modifying core beliefs - digging deeper than surface thoughts to change long-held beliefs like "I’m unlovable" or "I have to be perfect to be accepted."
- Behavioral activation - getting moving again. Depression drains energy. CBT helps you schedule small, meaningful activities to rebuild momentum.
- Exposure techniques - facing fears slowly and safely. For someone with social anxiety, this might mean starting with saying "hi" to a neighbor, then a coworker, then speaking up in a meeting.
- Skills training - learning communication, assertiveness, or relaxation techniques to handle tough situations.
- Relapse prevention planning - figuring out what might trigger a return to old patterns, and how to handle it.
- Homework assignments - CBT isn’t just during sessions. You practice skills between appointments. It’s like physical therapy for your mind.
Each session lasts 45 to 60 minutes. Most people attend 12 to 20 sessions total. That’s it. No years of therapy. No endless analysis.
What CBT Works For - And What It Doesn’t
CBT isn’t magic. But it’s one of the most effective treatments we have - and we know that because of science.
Over 2,000 randomized controlled trials have been done on CBT since 1977. That’s more than any other therapy. The National Institute for Health and Care Excellence (NICE) in the UK recommends it as a first-line treatment for:
- Depression
- Anxiety disorders (generalized anxiety, panic, social anxiety)
- Post-traumatic stress disorder (PTSD)
- Obsessive-compulsive disorder (OCD)
- Eating disorders
- Insomnia
- Chronic pain
For depression, CBT matches antidepressants in effectiveness - but with lower relapse rates. One study found that after 12 months, 52% of people who did CBT were in remission, compared to 47% on medication. And when they stopped treatment, only 24% of the CBT group relapsed, while 52% of the medication group did.
For anxiety? CBT beats other therapies. A 2012 meta-analysis found CBT had effect sizes of 0.77 to 1.14 - higher than other talk therapies.
But CBT isn’t perfect. It doesn’t work as well for:
- Severe trauma with complex PTSD - here, therapies like Dialectical Behavior Therapy (DBT) often do better.
- Children with serious behavioral issues - Parent-Child Interaction Therapy (PCIT) shows stronger results.
- People with severe cognitive impairment or acute psychosis - CBT requires thinking clearly and doing homework, which isn’t possible for everyone.

Real People, Real Results
Numbers don’t tell the whole story. Real people share what works.
One user on HealthUnlocked said graded exposure for social anxiety cut their panic attacks from 15 a week to 2. Another, with OCD, went from spending 4 hours a day washing hands to zero after 18 sessions of Exposure and Response Prevention - a CBT technique.
On Reddit’s r/mentalhealth, 78% of 1,420 posts about CBT were positive. People loved "thought records" - writing down situations, thoughts, and emotions to see patterns. "It felt like I was finally seeing my own mind," one person wrote.
But it’s not easy. CBT asks you to do work. Homework. Facing fears. Challenging beliefs that feel true. That’s why 32% of negative reviews mention frustration with assignments. And 27% say exposure exercises were emotionally hard at first.
The NHS surveyed 15,000 people who got CBT. 74% completed treatment. 68% said their symptoms improved. But for people with addiction on top of anxiety or depression, completion dropped to 58% - showing how complex mental health can be.
How to Get Started
You don’t need a referral to start CBT. In the UK, you can self-refer to NHS Talking Therapies. In the US, many insurance plans cover it. Private therapists typically charge £80-£150 per session.
But not all therapists are trained the same way. Look for someone certified by the Academy of Cognitive Therapy or trained by the Beck Institute. They’ve done 120-180 hours of training and supervised cases.
There are also digital tools. Apps like Woebot (FDA-cleared in 2021) use CBT principles to guide users through thought records and behavioral exercises. They’re not replacements for therapy - but they help between sessions or if you can’t access a therapist.
Free resources exist too. The National Alliance on Mental Illness (NAMI) offers downloadable CBT workbooks. Many libraries have them. YouTube has guided exercises. You can start learning today.
The Future of CBT
CBT isn’t stuck in the past. It’s evolving.
"Third-wave" CBT adds mindfulness and acceptance. Acceptance and Commitment Therapy (ACT) helps people live with pain instead of fighting it. For chronic pain, ACT shows 15% better results than traditional CBT.
Researchers are now using AI to analyze thought records in real time. Imagine an app that notices you’re using "all-or-nothing" thinking and gently asks, "Is that really true?"
The National Institute of Mental Health is testing "precision CBT" - matching treatment to brain patterns, not just symptoms. In 5-7 years, we might see CBT tailored to your biology.
But the core hasn’t changed. CBT works because it gives people control. It doesn’t promise quick fixes. It gives you tools. And tools last.
Is CBT Right for You?
Ask yourself:
- Do you want to change how you think and act - not just understand why you feel this way?
- Are you willing to do homework and practice skills outside of sessions?
- Do you have the mental capacity to reflect on your thoughts and challenge them?
If yes - CBT could be the most useful thing you do for your mental health this year.
If you’re unsure, try a free CBT workbook. Or talk to your GP. You don’t have to commit to 12 sessions to start learning. Just one step - one thought record - can begin to shift everything.