When you have type 2 diabetes, losing weight isn’t just about fitting into smaller clothes-it’s one of the most powerful tools you have to take back control of your health. In fact, losing just 5% of your body weight can slash your blood sugar levels, reduce your need for medication, and even push diabetes into remission. This isn’t wishful thinking. It’s science backed by decades of research, from the landmark Diabetes Prevention Program to real-life success stories from people just like you.
Why Weight Loss Matters for Diabetes
Extra fat, especially around your belly, doesn’t just sit there. It actively interferes with how your body uses insulin. That’s called insulin resistance. Your pancreas works harder to pump out more insulin, but over time, it gets worn out. That’s when blood sugar starts climbing. Losing weight reverses this. Less fat means your cells respond better to insulin, your pancreas gets a break, and your blood sugar naturally improves.
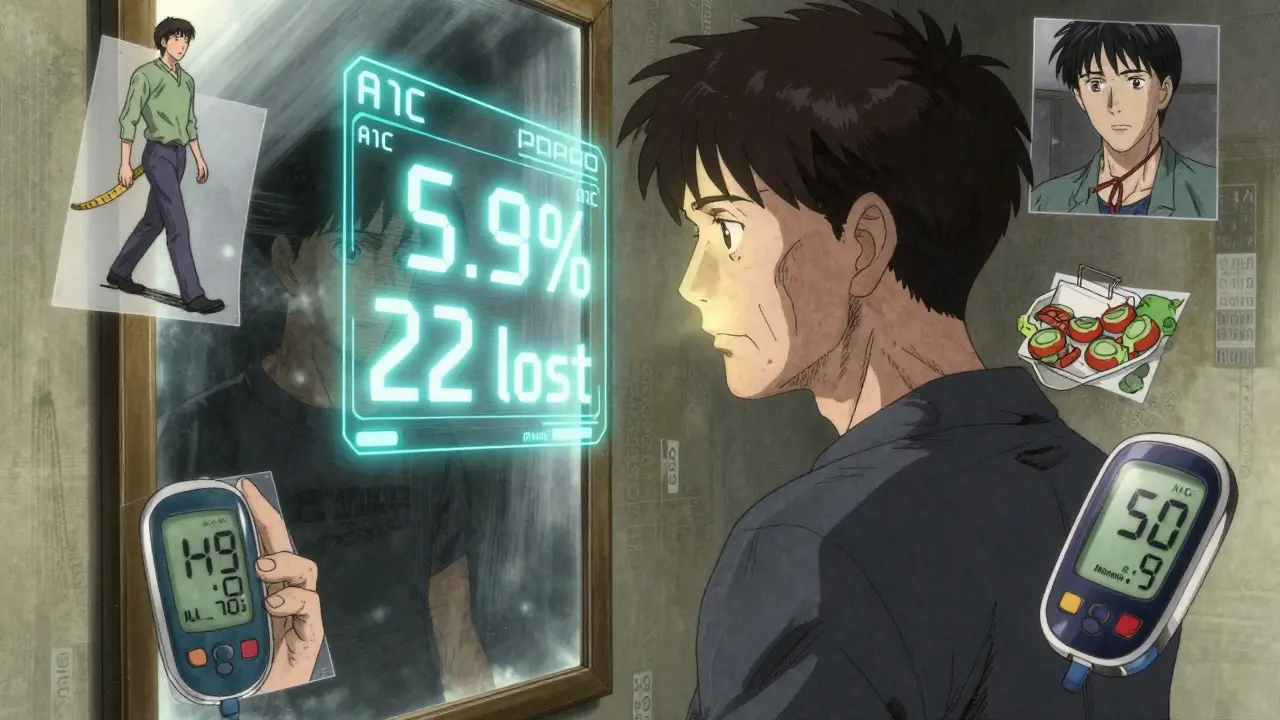
The numbers don’t lie. In the Diabetes Prevention Program, people with prediabetes who lost 5-7% of their body weight cut their risk of developing type 2 diabetes by 58%. That’s more effective than metformin. And for those already diagnosed, studies like DiRECT showed that losing 10 kg (about 22 lbs) led to diabetes remission in nearly half of participants after one year. Remission doesn’t mean a cure-it means your blood sugar is back to normal without medication. That’s life-changing.
How Much Weight Should You Aim to Lose?
You don’t need to lose 50 pounds to see results. Start small. Aim for 5-7% of your current weight. If you weigh 200 lbs, that’s 10-14 lbs. That’s it. That’s enough to drop your A1C by 0.5-1.0%, reduce blood pressure, and improve cholesterol.
Want bigger results? Go for 10-15%. That’s where many people start seeing diabetes remission. The DiRECT trial found that those who lost over 15 kg (33 lbs) had an 86% chance of remission. But here’s the catch: you don’t have to hit 15% right away. Start with 5%. Celebrate that. Then build from there.
Why not shoot for more? Because rapid, extreme weight loss can backfire-especially if you’re older or have had diabetes for a long time. It can increase fracture risk or cause dangerous drops in blood sugar if you’re on insulin or sulfonylureas. Slow and steady wins the race.
The Best Diet Approach for Weight Loss with Diabetes
There’s no magic diet. But some approaches work better than others when you’re managing diabetes.
The Mediterranean diet is a top choice. It’s rich in vegetables, beans, fish, olive oil, nuts, and whole grains. It’s not about cutting carbs completely-it’s about choosing the right ones. Fiber matters. Aim for at least 14 grams of fiber per 1,000 calories. That’s about 35-40 grams a day for most people. High-fiber foods fill you up, slow down sugar spikes, and feed good gut bacteria.
Portion control is non-negotiable. You can eat healthy foods and still gain weight if you eat too much. Use smaller plates. Measure your portions for a few weeks. Learn what a serving of rice or chicken actually looks like. Don’t eat straight from the bag. These small habits add up.
Protein helps too. It keeps you full longer and protects muscle as you lose fat. Include lean meats, eggs, tofu, Greek yogurt, and legumes at every meal. Avoid sugary drinks, even diet soda-studies link them to increased cravings and weight gain over time.
And yes, you can still enjoy your favorite foods. Just adjust the portions. A small slice of cake at a birthday party is fine. It’s the daily cookies, the late-night snacks, the sugary coffee that derail progress.

Exercise: It’s Not Just About Calories
You don’t have to run marathons. The goal is 150 minutes a week of moderate activity-like brisk walking, cycling, or swimming. That’s 30 minutes, five days a week. If you can’t do 30 at once, break it into 10-minute chunks. Every bit counts.
But here’s what most people miss: strength training. Lifting weights or doing bodyweight exercises (squats, push-ups, lunges) twice a week builds muscle. Muscle burns more calories at rest than fat. It also makes your body more sensitive to insulin. In one study, people who added strength training to their routine lost 2.5 times more belly fat than those who only walked.
Find something you actually like. If you hate the gym, dance in your living room. Take the dog for longer walks. Join a community walking group. If you enjoy it, you’ll stick with it.
Medications That Help (and Those That Don’t)
Your meds can help or hurt your weight loss efforts. Talk to your doctor about switching if you’re on something that causes weight gain.
Medications like metformin, GLP-1 agonists (semaglutide, tirzepatide), and SGLT2 inhibitors (dapagliflozin, empagliflozin) either help you lose weight or keep it off. Semaglutide (Wegovy) led to nearly 15% weight loss in trials. Tirzepatide (Mounjaro) hit over 20%.
On the flip side, insulin and sulfonylureas (like glimepiride) often cause weight gain and increase low blood sugar risk-especially when you’re eating less. If you’re trying to lose weight, ask your doctor if you can reduce these doses or switch to weight-neutral options. Never stop or change meds on your own.
Technology and Tools That Actually Work
Apps like MyFitnessPal, Noom, and MySugr help people track food, activity, and blood sugar. But the real win? Consistency. People who logged their meals daily lost 3.5-5.5% more weight than those who didn’t.
Continuous glucose monitors (CGMs) aren’t just for insulin users. Even if you’re not on insulin, seeing how your blood sugar reacts to food can be eye-opening. You’ll learn that oatmeal spikes you more than you thought. Or that a handful of almonds keeps you steady.
Telehealth coaching works too. The CDC’s National Diabetes Prevention Program offers virtual sessions with certified coaches. Participants who completed the full 16-week core program lost an average of 8% of their body weight. That’s more than most pills can deliver.

What Gets in the Way-and How to Beat It
Plateaus happen. You lose 10 lbs, then nothing for weeks. That’s normal. Your body adapts. Change your routine. Add more steps. Try a new workout. Cut back on hidden sugars in sauces or yogurt.
Emotional eating is the biggest barrier. Stress, boredom, sadness-it all leads to food. Keep a journal. Write down what you ate and how you felt before you ate it. You’ll start seeing patterns. Then find other ways to cope: walk, call a friend, listen to music, stretch.
Support matters. People who joined a group or had a buddy lost more weight and kept it off longer. Find your people. Online forums like r/diabetes or local meetups can help. You’re not alone.
And don’t ignore sleep. Poor sleep increases hunger hormones and makes cravings worse. Aim for 7-8 hours a night.
Real People, Real Results
One user on the American Diabetes Association’s forum lost 22 lbs in six months by walking 150 minutes a week and using portion control. Her A1C dropped from 7.2% to 5.9%. Another on Reddit lost 18 lbs with MyFitnessPal, but hit a wall until she added two days of strength training.
Not everyone succeeds with meds. One person tried semaglutide but couldn’t handle the nausea. She switched back to diet and movement-and lost 14 lbs anyway.
Success isn’t about perfection. It’s about showing up. Even on the days you eat too much or skip a workout. You get back up. You try again.
What Comes Next: Staying on Track
Losing weight is hard. Keeping it off is harder. That’s why maintenance is part of the plan. After you hit your goal, keep weighing yourself weekly. Keep moving. Keep eating mindfully. Keep your support system.
Studies show that people who stay in coaching programs for a year or more are far more likely to keep the weight off. The ADA recommends at least six maintenance sessions after the initial 16-week program. Don’t drop out when you’re close to the finish line.
Remember: this isn’t a diet. It’s a new way of living. One that gives you more energy, better sleep, fewer meds, and a future with fewer complications. That’s worth every step.




Tatiana Bandurina
January 21, 2026 AT 19:24Let me tell you, this post is textbook manipulation. They say losing 5% weight reverses diabetes like it’s some kind of magic trick. But they never mention that most people regain it within two years, and the metabolic damage just gets worse. The real issue is pharmaceutical greed pushing ‘remission’ as a marketing term while insulin prices keep soaring. You’re not cured-you’re just temporarily less sick while they profit.
Philip House
January 22, 2026 AT 15:59Interesting how this ignores the fact that insulin resistance isn’t just about fat-it’s about inflammation, gut microbiome disruption, and chronic stress. The Mediterranean diet helps, sure, but only if you’re not eating processed olive oil or ‘whole grain’ bread that’s 80% refined flour. Also, strength training isn’t optional. Muscle is your insulin sensitivity engine. If you’re not lifting, you’re just cardio-ing your way into a slower metabolism.
Jasmine Bryant
January 23, 2026 AT 14:55I’ve been doing this for 3 years now. Started at 210 lbs, A1C 8.1. Lost 18 lbs with just walking and cutting soda. My A1C is 5.7 now. No meds. The CGM was a game changer-I thought fruit was healthy until I saw my sugar spike after bananas. Also, sleep matters more than people say. I started sleeping 7.5 hours and stopped craving midnight snacks. It’s not rocket science, but it’s not easy either.
Sarvesh CK
January 24, 2026 AT 15:28It is imperative to recognize that the path to metabolic health is not merely a function of caloric restriction or physical exertion, but rather a holistic recalibration of one’s relationship with food, self, and societal norms. The modern paradigm of weight loss as a quantifiable metric fails to account for the psychosocial dimensions of chronic illness. True transformation arises not from adherence to protocols, but from the cultivation of self-compassion, sustained by community and mindful awareness. One must ask: are we seeking to heal, or merely to conform?
Brenda King
January 24, 2026 AT 15:54Love this. Seriously. I used to think I had to go keto to fix my diabetes. Turned out I just needed to stop eating cereal for breakfast. Now I eat eggs, spinach, and a handful of almonds. No counting. No apps. Just real food. My A1C dropped from 7.9 to 5.8 in 9 months. Also, walking after dinner? Game changer. My blood sugar stays flat. Thank you for not shaming people who aren’t perfect.
Neil Ellis
January 25, 2026 AT 23:39Man, this is the kind of post that makes me wanna hug a doctor. So many people think diabetes is just ‘eating too much sugar’-like it’s a moral failure. But this? This is science with soul. I’ve seen people turn their lives around with just 10 lbs lost and a daily walk. No miracle pills. No detox teas. Just consistency. And yeah, you can still have cake-just not every damn day. Celebrate the small wins. They add up.