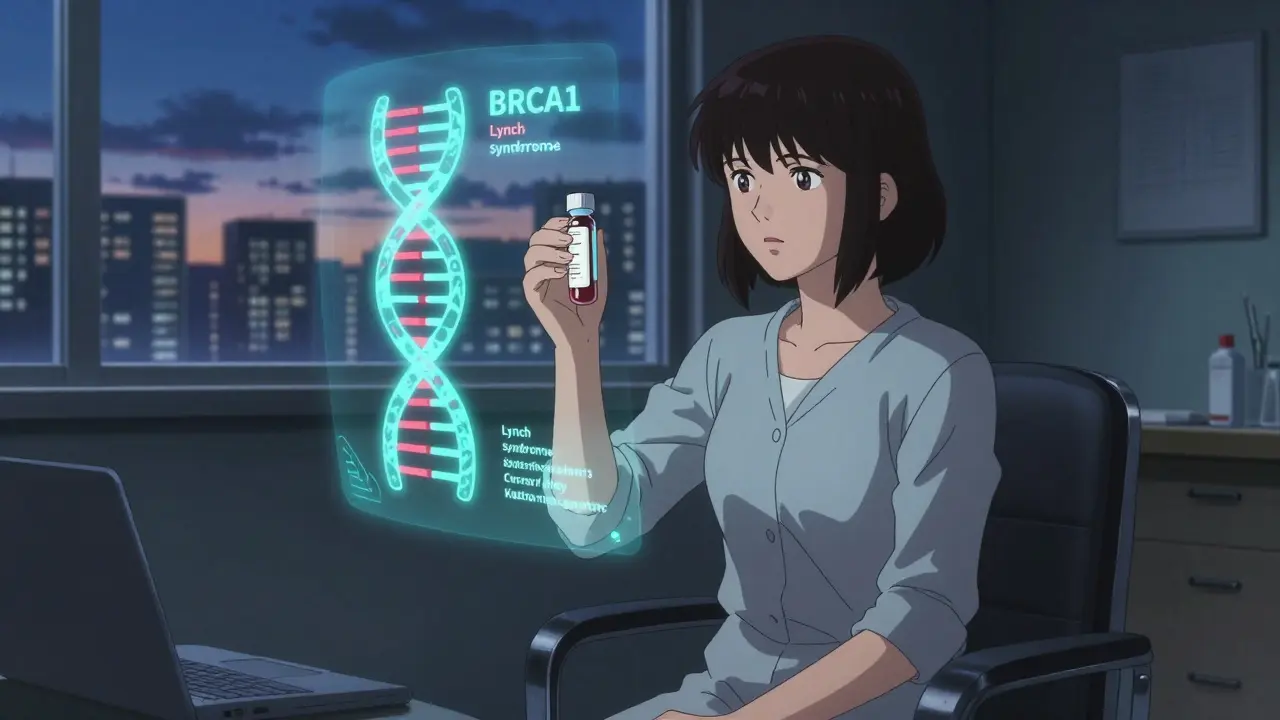
When you hear the word genetic testing, you might think of ancestry kits or fun DNA reports. But for people with a strong family history of cancer, it’s something far more serious-and potentially life-saving. Testing for inherited mutations like BRCA1, BRCA2, and Lynch syndrome genes isn’t about curiosity. It’s about knowing your risk before cancer starts, and taking steps to stop it.
What BRCA and Lynch Really Mean
BRCA1 and BRCA2 aren’t just names. They’re genes that help fix damaged DNA. When they’re broken by an inherited mutation, your body loses a major defense against cancer. Women with a harmful BRCA1 mutation have up to a 72% chance of developing breast cancer by age 80. For BRCA2, it’s around 69%. Ovarian cancer risk jumps to 44% for BRCA1 and 17% for BRCA2. Compare that to the general population’s 13% lifetime breast cancer risk and less than 2% for ovarian cancer.
Lynch syndrome is different. It’s not about breast or ovarian cancer-it’s about colorectal, endometrial, stomach, and other cancers. It’s caused by mutations in MLH1, MSH2, MSH6, PMS2, or EPCAM. Someone with Lynch has a 10% to 80% lifetime risk of colorectal cancer, depending on which gene is affected. That’s not a small chance. It’s a ticking clock.
These aren’t rare. About 1 in 400 people carry a BRCA mutation. Lynch syndrome affects 1 in 280. Most people don’t know they have it until someone in the family gets cancer young-or multiple family members get different cancers. That’s why testing matters.
How Testing Works Today
Forget testing just one gene. The standard now is a multigene panel. These tests look at 30 to 80 genes linked to cancer risk all at once. You give a blood or saliva sample. Labs use next-generation sequencing to scan your DNA for mutations. Results come back in about two to three weeks.
Companies like Myriad and Invitae run these tests with near-perfect accuracy-99.8% sensitive, 99.9% specific. But here’s the catch: not every change in your DNA is clearly good or bad. Some are called variants of uncertain significance, or VUS. That means scientists don’t yet know if it increases cancer risk or not.
That used to be a huge problem. In 2023, about 12.7% of BRCA2 test results showed a VUS. In February 2025, Mayo Clinic researchers published a breakthrough study using CRISPR to test nearly 7,000 BRCA2 variants. They reclassified 91% of them-turning uncertainty into clarity. For the DNA-binding region of BRCA2, VUS rates dropped from 12.7% to just 1.1%. That’s a game-changer for thousands of people who got confusing results before.
Why Panels Beat Single-Gene Tests
You might think: “If I’m worried about breast cancer, why test for colon cancer genes?” Because cancer doesn’t care about your assumptions.
A 2023 study of over 38,000 people found that testing only BRCA1 and BRCA2 missed 30% to 50% of actionable mutations. People walked away thinking they were safe-when they actually carried a dangerous mutation in PALB2, ATM, or CHEK2. These genes are now part of the NCCN’s top-tier list of clinically useful genes as of 2025.
Single-gene tests have lower VUS rates (around 2.3%), but they’re blind to the bigger picture. Multigene panels, while increasing VUS rates to about 7.8%, find far more real threats. The trade-off is worth it. Finding a Lynch mutation in a 42-year-old with colon cancer led to immunotherapy with pembrolizumab-and complete remission, according to a 2025 Fred Hutchinson case study.
What Direct-to-Consumer Tests Don’t Tell You
23andMe offers a BRCA test. It sounds convenient. But it only checks for three specific mutations common in people of Ashkenazi Jewish descent. That’s it. For everyone else-97% of the population-it misses nearly every harmful BRCA variant. A 2024 NEJM study showed that 97% of pathogenic BRCA mutations in non-Ashkenazi individuals are invisible to these tests.
And it gets worse. These tests don’t include Lynch genes. They don’t cover PALB2, CHEK2, or ATM. You get a false sense of security. One woman in a 2025 Reddit thread shared that she tested negative on 23andMe, skipped medical screening, and was diagnosed with stage 3 ovarian cancer at 34. Her family had multiple cases. She never knew she was at risk.
Don’t use DTC tests for medical decisions. Ever.

Who Should Get Tested
Not everyone needs this. But if any of these apply to you, talk to your doctor:
- You were diagnosed with breast cancer before age 50
- You have ovarian, pancreatic, or metastatic prostate cancer at any age
- Multiple close relatives have breast, ovarian, colorectal, or endometrial cancer
- A family member tested positive for a hereditary cancer mutation
- You’re of Ashkenazi Jewish descent and have any family history of breast, ovarian, or pancreatic cancer
The National Comprehensive Cancer Network (NCCN) guidelines are clear: if you meet these criteria, you should get a multigene panel test. Not a single-gene test. Not a DTC kit. A full panel, ordered through a medical provider.
The Critical Role of Genetic Counseling
Testing without counseling is dangerous. You could misunderstand your results. You might panic over a VUS. Or worse-you might ignore a positive result because you didn’t understand what it meant.
Before testing, you need a 60- to 90-minute session with a certified genetic counselor. They’ll map your family history, explain what each gene means, and help you weigh the emotional and medical consequences. After testing, they’ll interpret your results and help you decide on next steps: more frequent screenings, preventive surgeries, or targeted treatments.
Yet, only 87% of U.S. cancer centers meet this standard. In community clinics, it’s even lower. Many doctors still order tests without counseling. That’s a gap. And it’s putting lives at risk.
What Happens After a Positive Result
Finding a mutation isn’t a death sentence. It’s a heads-up.
For BRCA carriers:
- Women can start breast MRI and mammograms at age 25
- Prophylactic mastectomy reduces breast cancer risk by up to 95%
- Removal of ovaries and fallopian tubes by age 35-40 cuts ovarian cancer risk by 80% and breast cancer risk by 50%
For Lynch syndrome carriers:
- Colonoscopies every 1-2 years starting at age 20-25
- Endometrial biopsies annually for women
- Aspirin daily (shown to reduce colorectal cancer risk by up to 60% in Lynch patients)
And here’s the biggest win: if you have a mutation and get cancer, your treatment changes. PARP inhibitors like olaparib work wonders for BRCA-related breast and ovarian cancers. Immunotherapy works better for Lynch-related tumors. Genetic testing doesn’t just prevent cancer-it makes treatment more effective.

The Hidden Costs and Risks
Medicare and most private insurers cover testing if you meet NCCN criteria. Approval rates are 98.7%. But out-of-pocket costs for self-pay patients can hit $450. And if you need a retest because your VUS got reclassified? Myriad charges $250 for that update. Some patients can’t afford it.
Then there’s insurance discrimination. GINA protects you from health insurance discrimination based on genetic results. But it doesn’t cover life, disability, or long-term care insurance. A 2024 survey found 9% of people who tested positive reported being denied coverage or charged higher premiums.
And VUS still cause anxiety. One in five people report significant stress after getting a VUS result-even when told it’s likely harmless. That’s why follow-up counseling matters.
What’s Next for Genetic Testing
The future is brighter. Stanford researchers identified 380 gene-regulating variants linked to cancer risk across 13 types. These aren’t single-gene mutations-they’re subtle switches that nudge your risk up or down. Soon, we’ll combine them into polygenic risk scores. Imagine knowing your cancer risk isn’t just from one broken gene, but from dozens of small genetic tweaks.
And the push is on to test everyone with cancer. A 2025 ASCO survey found 67% of oncologists support universal germline testing for all cancer patients. Why? Because finding a mutation doesn’t just help you-it helps your whole family. Cascade testing (testing relatives after a positive result) is the most cost-effective cancer prevention tool we have.
But it won’t work unless access improves. Black patients are tested at less than half the rate of white patients. Community clinics still lag behind academic centers. We need better training for doctors, better funding for counseling, and more equitable access.
Final Thoughts
Genetic testing for cancer risk isn’t about fear. It’s about power. The power to act before cancer starts. The power to choose prevention over treatment. The power to protect your children and siblings.
If you have a family history of cancer, don’t wait for a diagnosis to get tested. Talk to your doctor. Ask for a referral to a genetic counselor. Get a multigene panel. Don’t settle for a DTC test. Don’t skip counseling.
Knowing your genes doesn’t mean you’ll get cancer. It means you’ll know how to stop it.
Who should consider genetic testing for cancer risk?
Anyone with a personal or family history of early-onset cancer (before 50), multiple related cancers in close relatives, or known hereditary cancer mutations in the family. People of Ashkenazi Jewish descent with any family history of breast, ovarian, or pancreatic cancer should also consider testing. The NCCN guidelines outline specific criteria for who qualifies.
Can I just use a 23andMe or AncestryDNA test for cancer risk?
No. Direct-to-consumer tests like 23andMe only screen for three specific BRCA mutations common in Ashkenazi Jewish populations. They miss over 97% of harmful BRCA variants in other groups and don’t test for Lynch syndrome or other high-risk genes. These tests are not medically reliable and should never be used to make health decisions.
What if my test shows a variant of uncertain significance (VUS)?
A VUS means scientists don’t yet know if the gene change increases cancer risk. It’s not positive or negative. Most VUS are eventually reclassified as benign. Since early 2025, research from Mayo Clinic has drastically reduced VUS rates in BRCA genes-from over 12% down to under 1.5% in key regions. You should get follow-up counseling and consider retesting in 1-2 years as knowledge improves.
Does insurance cover genetic testing?
Yes, if you meet NCCN guidelines. Medicare covers testing with a 98.7% approval rate. Most private insurers do too. Out-of-pocket costs for self-pay patients range from $250 to $450. Some labs charge extra for reclassification updates. GINA protects against health insurance discrimination, but not life, disability, or long-term care insurance.
Will testing change my treatment if I already have cancer?
Absolutely. If you have a BRCA mutation and develop breast or ovarian cancer, you may benefit from PARP inhibitors like olaparib, which are more effective in these cases. If you have Lynch syndrome and colorectal cancer, immunotherapy drugs like pembrolizumab often work better. Testing can guide your treatment choices and improve outcomes.
Can I be denied insurance because of my genetic test results?
Under GINA, health insurers and employers cannot use your genetic test results to deny coverage or employment. However, GINA does not cover life insurance, disability insurance, or long-term care insurance. Some people have reported being denied or charged more for these types of policies after a positive result. It’s important to understand these limits before testing.




Jeffrey Hu
January 8, 2026 AT 23:56Look, I get it - multigene panels are the gold standard. But let’s be real: most primary care docs don’t know the difference between BRCA and Lynch. I’ve seen patients get ordered a 70-gene panel by a GP who thinks ‘PALB2’ is a new iPhone model. Counseling? Ha. They hand you a PDF and say ‘call if you have questions.’ That’s not medicine - that’s genetic Russian roulette.
RAJAT KD
January 10, 2026 AT 04:46Testing saved my sister’s life. She had no symptoms, just a mom with early ovarian cancer. Found BRCA1 at 29. Had prophylactic surgery. Now she’s 35 and cancer-free. Don’t wait for symptoms. Know your genes.
Meghan Hammack
January 12, 2026 AT 04:36I’m a nurse and I’ve seen too many women panic over a VUS. One lady cried for 20 minutes because her report said ‘uncertain significance’ - she thought it meant ‘you’re gonna die.’ We spent an hour explaining it’s like a ‘maybe’ on a test, not a death sentence. Counseling isn’t optional - it’s oxygen.
Micheal Murdoch
January 13, 2026 AT 21:36There’s a quiet revolution happening here. Five years ago, a VUS meant years of anxiety and guesswork. Now, with CRISPR-based functional assays, we’re turning confusion into clarity. That 91% reclassification rate from Mayo? That’s not just science - that’s hope being coded into DNA. We’re moving from ‘maybe’ to ‘know.’ And that changes everything for families who’ve lived in the shadow of cancer for generations.
It’s not just about mastectomies or colonoscopies. It’s about giving people back their future. Imagine knowing you won’t lose your kids to the same disease that took your mom. That’s not medical tech - that’s legacy protection.
And yes, DTC tests are dangerously misleading. I had a patient who tested ‘negative’ on 23andMe, skipped screening, and got stage 4 ovarian cancer at 32. Her family had seven cancers across three generations. She thought she was safe because a consumer test said so. That’s not negligence - it’s a systemic failure.
Insurance coverage is good, but GINA’s loopholes are terrifying. I’ve seen people decline testing because they’re afraid they’ll get denied life insurance. That’s the real cost of genetic knowledge - it’s not money. It’s fear. We need policy reform as urgently as we need better labs.
The future? Polygenic risk scores. Not one broken gene, but dozens of tiny nudges adding up. That’s where we’re headed. But we can’t leave people behind while we wait for the future. Right now, a multigene panel + counselor = power. Don’t settle for less.
Heather Wilson
January 14, 2026 AT 12:28Why are we acting like genetic testing is some miracle cure? It’s expensive, emotionally devastating, and often leads to unnecessary surgeries. I’ve seen women get mastectomies because of a VUS - and then find out five years later it was benign. This isn’t empowerment - it’s fear-driven medicine.
And don’t get me started on the ‘cascade testing’ hype. You test one person, then you drag their entire family into a medical nightmare. What about privacy? What about consent? This is eugenics light, dressed up as prevention.
Most cancers are caused by environment and lifestyle. Blaming DNA is lazy. Stop selling fear as science.
Chris Kauwe
January 16, 2026 AT 12:04Let’s cut through the biotech buzzwords. BRCA? Lynch? These are just fancy labels for inherited mutations - nothing more. The real issue is that Big Pharma and genetic testing conglomerates like Myriad have turned risk assessment into a profit engine. They push panels because they make money off retesting VUS. The science is real, but the incentives are corrupt.
And don’t tell me GINA protects you. It doesn’t. I know a guy who got denied $2M in life insurance after a BRCA2 positive. He’s still paying 300% higher premiums. This isn’t healthcare - it’s genetic redlining.
Also, why is everyone ignoring the fact that 70% of breast cancers occur in women with NO family history? We’re hyper-focusing on a tiny subset while ignoring the majority. This is misallocated resources disguised as progress.
Ian Long
January 16, 2026 AT 17:35I get the fear. I’ve sat with people who just got their BRCA+ result and couldn’t speak for an hour. But here’s the truth: knowledge doesn’t kill. Ignorance does.
I’m not saying it’s easy. I’m saying it’s worth it. My cousin got a Lynch diagnosis at 38. Started colonoscopies every year. Found a polyp. Removed it. No cancer. She’s 42 now. Alive. Because she didn’t wait.
And yeah, VUS sucks. But the Mayo study? That’s the kind of progress that turns panic into peace. We’re not perfect yet - but we’re getting better. Faster than ever.
Stop equating testing with doom. It’s not a death sentence. It’s a head start.
Alicia Hasö
January 17, 2026 AT 05:51TO EVERYONE WHO SAYS "DON'T TEST BECAUSE IT'S TOO STRESSFUL" - I have three words for you: MY SISTER WAS 31. She had triple-negative breast cancer. No family history. No warning. She died six months later. If she’d known she carried a BRCA2 mutation - even if she didn’t know it was there - she could’ve had a prophylactic mastectomy. She could’ve lived to see her daughter turn 10.
This isn’t about fear. It’s about love. It’s about giving the people you care about a fighting chance. If you have a family history - GET TESTED. Not tomorrow. Not next year. NOW. Because cancer doesn’t wait. And neither should you.
And if you’re scared of the cost? Ask for financial aid. Most labs have programs. Ask for sliding scale. Ask for help. You are not alone. And you are not powerless.
Darren McGuff
January 18, 2026 AT 11:09Just a quick note from the UK - we’ve had NICE guidelines for this since 2019. If you meet criteria, you get a multigene panel free on the NHS. Genetic counseling? Mandatory. No exceptions. We’re not perfect, but we’re ahead of the US on access. Shame more Americans don’t know this isn’t a luxury - it’s standard care.
Also, the 97% miss rate on 23andMe? That’s not just misleading - it’s unethical. Companies should be held liable for false reassurance. People are dying because of this.
Aron Veldhuizen
January 18, 2026 AT 16:53Oh wow, another ‘genetic testing is the answer’ sermon. Let me guess - you also think vaccines are a miracle and masks save lives? Wake up. We’re being manipulated by corporate-funded science. The real cause of cancer? Toxins, processed food, glyphosate, EMFs. Your DNA is fine - your environment is poisoned.
Why are we obsessing over genes when the air we breathe and the water we drink are full of carcinogens? This is distraction therapy. They want you to blame your ancestors, not the corporations dumping chemicals into the soil.
And don’t even get me started on ‘PARP inhibitors.’ Another overpriced drug that only extends life by a few months. We’re treating symptoms, not causes. This whole system is broken.
Drew Pearlman
January 19, 2026 AT 00:40I just want to say - if you’re reading this and you’re scared to get tested, I get it. I was terrified too. I had two aunts with breast cancer, one at 34, another at 39. I delayed testing for three years because I didn’t want to know. I thought if I didn’t know, I couldn’t be doomed.
Then I read about a woman who got her results on a Friday, had surgery on Monday, and was back at her kid’s soccer game by Wednesday. She said, ‘I didn’t lose my breasts - I saved my life.’ That stuck with me.
I got tested last year. BRCA2 positive. Had the surgeries. It wasn’t easy. But I’m alive. My kids have a mom. My husband has a wife. And I didn’t wait until it was too late.
You don’t have to be brave. You just have to be ready to choose life. And that’s enough.
Matthew Maxwell
January 19, 2026 AT 22:44It’s morally irresponsible to promote genetic testing without first addressing the elephant in the room: eugenics. We’ve spent decades trying to eliminate ‘bad genes.’ Now we’re doing it with a lab coat and insurance forms. This isn’t prevention - it’s selective reproduction disguised as healthcare.
What happens when we start screening embryos? When insurers demand gene edits? When ‘high-risk’ becomes a social stigma? We’re not saving lives - we’re engineering a new class of genetic inferiority.
And don’t pretend GINA fixes anything. It doesn’t protect against social discrimination. People with BRCA mutations are already being passed over for promotions, treated as liabilities. This isn’t science. It’s social engineering.
Lindsey Wellmann
January 21, 2026 AT 20:22okay so i just got my BRCA1+ results and i’m crying but also kinda relieved?? like… i’m 28 and i’ve watched my mom go through chemo 3 times. i didn’t want to know because i thought it would ruin my life. but now? now i can ACT. i’m doing the mastectomy next month. i’m getting my tubes out. i’m not waiting. i’m choosing me. and if you’re scared? you’re not alone. but you’re also not powerless. 💕🫂 #genetictestingisnotafate #chooseyourfuture
Ashley Kronenwetter
January 21, 2026 AT 20:26As a genetic counselor, I want to emphasize: testing without pre-test counseling is a violation of ethical standards. The emotional impact of a positive result - or even a VUS - can be profound. Patients need time, space, and support to process what this means for them and their family. This is not a lab report. It’s a life-altering revelation. If your provider skips counseling, ask for a referral. Insist on it. Your future self will thank you.
Micheal Murdoch
January 23, 2026 AT 11:24Just read the comment from @6672 - that’s why this matters. Not the stats. Not the VUS rates. Not the insurance loopholes. It’s that moment when someone realizes they’re not just a patient - they’re a protector. That’s the real power. Not the gene. The choice.
And to the person who said this is eugenics - you’re missing the point. We’re not eliminating people. We’re giving them control. No one is being forced. No one is being erased. We’re just giving people the tools to choose their own path. That’s not eugenics. That’s autonomy.