Every year, the FDA issues hundreds of drug safety communications - notices that can change how doctors prescribe medications and how patients take them. These aren’t recalls. They’re not panic alerts. But they’re some of the most important updates you’ll never hear about unless you’re looking for them.
What Exactly Is a Drug Safety Communication?
A Drug Safety Communication (DSC) is an official notice from the U.S. Food and Drug Administration that tells doctors, pharmacists, and patients about new safety information on a medicine that’s already on the market. These aren’t warnings about bad batches or manufacturing mistakes. They’re about risks that only show up after thousands - sometimes millions - of people have taken the drug.
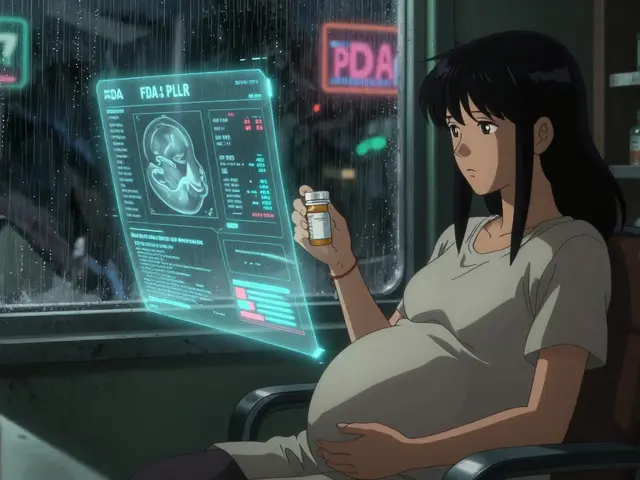
Think of it this way: when a drug gets approved, the FDA has data from clinical trials. Those trials involve a few thousand people over months or a couple of years. But real life? Millions of people take the drug for years. Some are older. Some have other illnesses. Some take five other pills at the same time. That’s when hidden risks show up.
The FDA uses data from its own systems - like the MedWatch program where doctors and patients report side effects - plus studies from hospitals, insurance claims, and even electronic health records. When something pops up that could change the balance between a drug’s benefits and its dangers, they issue a DSC.
How Do These Communications Work?
Every DSC follows a clear structure. It starts with: What safety concern is the FDA announcing? Then it breaks down: Recommendations for healthcare professionals and Recommendations for patients. Finally, there’s Additional Information - usually a summary of the data behind the warning.
For example, in July 2025, the FDA issued a DSC about long-acting opioid painkillers. The message: long-term use increases the risk of addiction, misuse, and fatal overdose. The recommendation? Manufacturers had to update labels to warn about this. Doctors were told to avoid prescribing these for chronic pain unless absolutely necessary. Patients were told to talk to their doctor before continuing use.
These aren’t vague suggestions. They’re based on real data. In the opioid case, the FDA reviewed studies showing a 40% higher risk of overdose among patients using ER/LA opioids for more than 90 days. That’s not a small number.
Why Do They Take So Long?
It used to take an average of 2.6 years from the time a safety signal was spotted to when the FDA issued a DSC. That meant people were exposed to risks for years before anyone knew.
That’s changing. Thanks to new AI tools that scan millions of patient records automatically, the average time dropped to 1.8 years in 2025. The FDA is also starting to share information earlier - even while they’re still studying the data. So now you might see a DSC that says: “We’re seeing possible signs of liver injury with Drug X. We’re still investigating. Here’s what we know so far.”
That’s a big shift. In the past, the FDA waited until they were 95% sure before speaking. Now, they’re saying: “Here’s what we’re seeing. Be alert.”
Who Gets These Alerts?
Healthcare professionals are the main target. Hospitals, pharmacies, and clinics are supposed to track these. The American Society of Health-System Pharmacists found that 68% of hospital pharmacists check the FDA’s Drug Safety page every week. Only 42% of community pharmacists do. That gap matters. A patient might get a new prescription at a local pharmacy that hasn’t seen the latest warning.
Electronic health record systems like Epic and Cerner are supposed to auto-alert doctors when a DSC comes out. But a 2024 study found only 58% of these systems properly flag the urgency level. So a doctor might see a warning about a rare but deadly reaction - and miss it because the system labeled it as “low priority.”
Patients? They usually find out through their doctor, a pharmacist, or a news article. The FDA now includes plain-language patient advice in 47% of DSCs - up from 28% in 2018. That’s progress. But most patients don’t know where to look. The FDA’s Drug Safety page isn’t easy to navigate unless you know exactly what you’re searching for.
Real Impact: When a DSC Changes Practice
There are clear cases where DSCs saved lives.
In 2023, a DSC warned that the antidepressant citalopram could cause dangerous heart rhythm changes in older adults - especially at doses above 20 mg. A geriatrician in Boston told her team: “Stop prescribing anything over 20 mg for patients over 65.” Within six months, arrhythmias in that group dropped by 32%.
Another example: proton pump inhibitors (PPIs) like omeprazole. A 2022 DSC linked long-term use to a higher risk of C. diff infection. A 2023 FDA survey found that 73% of patients who heard about this talked to their doctor. But only 38% actually stopped or switched the drug. Why? Because heartburn is annoying. And the infection risk feels distant. That’s the challenge: changing behavior isn’t just about information - it’s about fear, habit, and access.

What’s Changing in 2025 and Beyond?
The volume of DSCs is rising fast. In 2008, the FDA issued 42. In 2024, they issued 187. That’s a 345% increase. Why? Because the tools to detect risks have gotten better. The FDA’s Sentinel Initiative now monitors data from 300 million patient records across 16 health systems. That’s like having a national early-warning system for drug safety.
Also, new kinds of drugs are coming - gene therapies, cell therapies, AI-powered diagnostics. These are complex. Their risks aren’t always obvious. That means more DSCs, not fewer.
The FDA’s 2025-2027 plan says they want to cut the time between detecting a risk and issuing a DSC by 25%. They’re also testing a new system that will push alerts directly into patient portals - so if you’re on a drug with a new warning, your MyChart account might pop up a note: “Your doctor has been notified about a possible risk with your medication.”
What Should You Do?
If you take any prescription medication - especially if you’re on more than one - you need to know about DSCs. Here’s how:
- Ask your doctor or pharmacist: “Have there been any new safety updates on my meds?”
- Check the FDA’s Drug Safety Communications page. Filter by your drug name or specialty (cardiology, diabetes, mental health).
- Sign up for FDA email alerts. Over 147,000 healthcare pros are subscribed. You don’t need to be a professional to get them.
- Don’t panic if you see a DSC. Read the patient recommendations. Talk to your provider. Don’t stop your medicine unless they tell you to.
Some drugs are worth the risk. Others aren’t. DSCs help you know the difference.
Why This Matters More Than You Think
Most people think drug safety ends when a pill gets approved. It doesn’t. It’s just starting. The real test is what happens when millions of people use it for years. That’s where DSCs come in - they’re the system’s way of saying: “We’re still watching. We’re still learning.”
And that’s the quiet power of post-marketing surveillance. It’s not flashy. It doesn’t make headlines. But it’s the reason you’re safer today than you were ten years ago.
Are FDA Drug Safety Communications the same as drug recalls?
No. A drug recall means the product is pulled from shelves because of contamination, mislabeling, or manufacturing defects. A Drug Safety Communication is about new safety risks discovered after the drug has been used widely. The drug stays on the market, but its use may change - like lower doses, new warnings, or restrictions for certain patients.
Can I trust FDA Drug Safety Communications?
Yes. The FDA bases these on real-world data from millions of patients, not just lab studies or small trials. They use multiple sources - adverse event reports, health insurance claims, hospital records, and even AI analysis of electronic health records. While no system is perfect, the FDA’s process is one of the most rigorous in the world. They don’t issue these lightly.
What should I do if I see a DSC about my medication?
Don’t stop taking it. Read the patient recommendations carefully. Then call your doctor or pharmacist. Ask: “Does this apply to me? Should I change anything?” Many DSCs recommend monitoring - like blood tests or checking for new symptoms - rather than stopping the drug. Your provider can help you weigh the risks and benefits for your situation.
Do DSCs only affect prescription drugs?
Mostly, yes. The FDA’s Drug Safety Communications focus on prescription and some over-the-counter drugs that require careful use - like high-dose NSAIDs, certain sleep aids, or long-term antibiotics. They don’t cover dietary supplements, cosmetics, or medical devices. Those have separate reporting systems.
How often are DSCs issued?
The number has grown sharply. In 2024, the FDA issued 187 Drug Safety Communications - up from 42 in 2008. That’s more than 3 per week. The trend is expected to continue, with projections of 210-230 per year by 2027, as more complex drugs enter the market and surveillance tools improve.
Why don’t I hear about DSCs in the news?
Most DSCs don’t make headlines because they’re targeted. They’re not about a single drug causing mass harm - they’re about specific risks in specific groups. For example, a warning about a heart rhythm risk in elderly patients with kidney disease won’t grab national attention. But it’s life-changing for those affected. The FDA publishes them directly so the right people - doctors and patients - can act, without causing unnecessary panic.



kenneth pillet
January 19, 2026 AT 06:55Been on a few of these meds long term. Never knew the FDA even tracked this stuff. Good to know they're still watching.
Jodi Harding
January 20, 2026 AT 18:35They wait until people die before they say anything. That's not safety. That's damage control.
Danny Gray
January 22, 2026 AT 07:03So let me get this straight - the FDA spends billions on drugs, then waits years to admit they might kill you? Sounds like a business model, not a public health system.
Tyler Myers
January 23, 2026 AT 02:37AI scanning patient records? Yeah right. That’s just Big Pharma feeding them data to keep the pills flowing. The real danger? They’re letting the same companies who made the drug *help* analyze the risks. Conflict of interest? More like conflict of profit.
Kristin Dailey
January 24, 2026 AT 21:22Why don’t they just ban the bad ones instead of writing essays? We don’t need warnings. We need action.
Aysha Siera
January 26, 2026 AT 08:19They’re using AI? That’s how they track us. Your pills are watching you. Your EHR is a spy tool. This isn’t safety - it’s surveillance dressed as care.