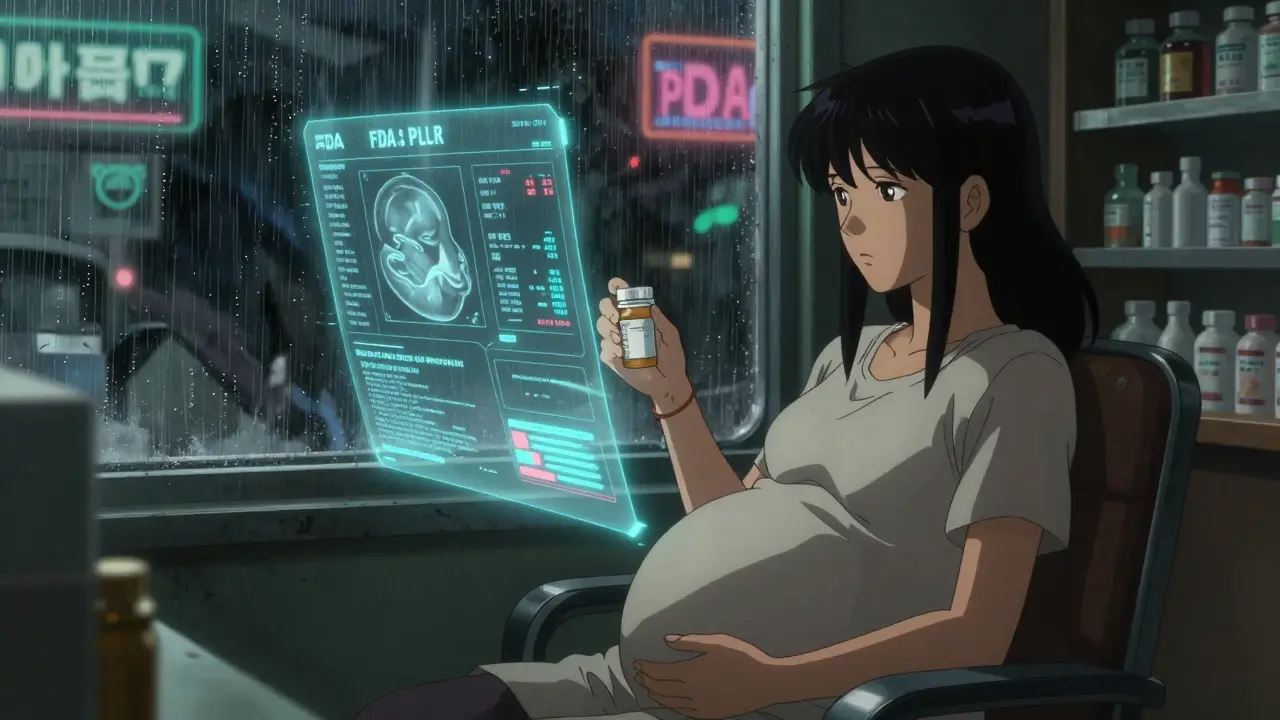
PLLR Drug Safety Assessment Tool
How to Use This Tool
Enter key details from your medication's PLLR label to assess pregnancy and lactation safety. This tool helps interpret the new FDA labeling system but doesn't replace medical advice.
Safety Assessment Results
When you’re pregnant or breastfeeding, taking any medication isn’t just about what works-it’s about what’s safe. For decades, doctors relied on simple letters-A, B, C, D, X-to decide if a drug was okay during pregnancy. But those letters didn’t tell the whole story. In fact, they often confused more than they helped. That’s why the FDA changed the rules. In December 2014, they rolled out the Pregnancy and Lactation Labeling Rule (PLLR), replacing outdated letter grades with clear, detailed sections that actually help you make informed choices.
What the PLLR Replaced-and Why It Was Broken
Before the PLLR, every prescription drug label had a pregnancy category: A, B, C, D, or X. Category A meant "safe." Category X meant "don’t take-it causes birth defects." Simple, right? Not really. The problem was that these categories were based on limited data. A drug with no human studies but no animal harm got a B. A drug with clear risks in humans but no animal data got a C-even if the human risk was higher. That created a dangerous illusion: if a drug had no known harm, it was assumed safe. But what if no one had studied it? That’s not safety-that’s ignorance. Doctors started ignoring the letters. Patients got conflicting advice. One provider said, "It’s Category B, so it’s fine." Another said, "We don’t know enough." The system wasn’t just outdated-it was misleading.The Three New Sections: What You Need to Know
The PLLR didn’t just tweak the labels. It rebuilt them. Now, every prescription drug has three focused subsections under Section 8: Pregnancy, Lactation, and Females and Males of Reproductive Potential. Let’s break down what each one actually tells you.Pregnancy: Risk Summary, Clinical Considerations, Data
The Pregnancy section doesn’t say "safe" or "unsafe." It says:- Risk Summary: What do we know about harm to the fetus? Is there a link to heart defects, low amniotic fluid, or developmental delays? This isn’t vague-it’s specific. For example, one drug’s label now says: "Discontinuation led to a rise in amniotic fluid index; restarting caused it to drop again." That’s real clinical detail.
- Clinical Considerations: When during pregnancy is exposure most risky? Does the dose need to change? What about labor and delivery? What if you’re already taking it when you find out you’re pregnant? This section answers those questions.
- Data: Where did this info come from? Animal studies? Human case reports? Pregnancy registries? This part shows you the evidence-not just the conclusion.
Lactation: What Goes Into Breast Milk?
Breastfeeding moms used to get one line: "Use with caution." Now they get real numbers. The Lactation section tells you:- How much of the drug ends up in breast milk compared to the mother’s blood.
- Whether it affects milk production.
- What the baby might experience-drowsiness, poor feeding, or no effect at all.
Females and Males of Reproductive Potential: Planning Ahead
This section wasn’t in the old system. Now, it’s required. It answers:- Do you need a pregnancy test before starting this drug?
- What kind of birth control is recommended? (Not just "use contraception"-but which methods interact with the drug?)
- Could this drug affect fertility in men or women?
Why This Matters More Than You Think
About 6 million pregnancies happen in the U.S. every year. On average, each pregnant woman takes three to five prescription drugs. Some are for chronic conditions like epilepsy, depression, or diabetes. Others are for infections or pain. Before PLLR, doctors often avoided prescribing anything-just in case. Now, they can say: "Here’s what we know. Here’s what we don’t. Here’s what to watch for." That’s a huge shift. Take SSRIs, for example. In the old system, most were Category C. Many women stopped them cold during pregnancy, risking severe depression. With PLLR, labels now show that the risk of untreated depression may be greater than the risk of the medication. That context changes everything.
What’s Missing-and What’s Still Confusing
The PLLR fixed a lot, but it didn’t fix everything. For one, there’s no standardized way to say "high risk" or "low risk." One label might say "potential risk," another might say "adverse effects observed." That’s intentional-the FDA didn’t want to create new oversimplifications. But it means you have to read carefully. Also, the rule doesn’t cover over-the-counter drugs, supplements, or herbal products. If you’re taking melatonin, ibuprofen, or prenatal vitamins, you still need to ask your provider. And while the FDA requires manufacturers to update labels when new data comes in, not all updates happen fast. A drug’s label might still reflect data from five years ago. Always check the most recent version.How to Use PLLR Labels in Real Life
You don’t need to be a doctor to use this. Here’s how:- Find the drug’s official prescribing information. Go to drugs.com or the FDA’s website. Search by brand or generic name.
- Open the "Use in Specific Populations" section (Section 8).
- Read the Risk Summary first. Look for specific outcomes: "increased risk of neural tube defects," "reduced fetal growth," etc.
- Check the Clinical Considerations. Is timing important? Does dose matter? Are there monitoring requirements?
- Look for pregnancy registries. If one exists, you can enroll. That helps future moms.
- For breastfeeding: See the milk levels. If the drug is below 10% of maternal dose and no infant side effects are reported, it’s likely compatible.
International Differences: FDA vs. EMA
The U.S. isn’t alone in this. The European Medicines Agency (EMA) has its own system. But here’s the catch: in 68% of cases, the FDA and EMA describe the same drug’s pregnancy risk differently. One drug might be labeled "avoid" in Europe but "consider use" in the U.S. Why? Different data interpretations. Different risk thresholds. Different cultural norms. If you’re traveling, moving, or getting a drug from abroad, check both labels. Don’t assume they match.What’s Next for PLLR?
The rule is still evolving. More drugs are being updated. More registries are being created. More data is being collected from real-world use. The FDA now encourages manufacturers to include data on long-term child development outcomes-something that wasn’t required before. And there’s growing pressure to harmonize with other countries, even if it’s slow. For now, the PLLR is the most detailed, evidence-based system for pregnancy and breastfeeding drug safety in the world. It doesn’t give you easy answers. But it gives you the right questions to ask.Are all prescription drugs updated with PLLR labels?
Yes, all prescription drugs and biologics approved after June 30, 2001, must use PLLR labels. Older drugs were required to remove the old A-B-C-D-X categories by 2017 and transition to the new format. If you’re unsure, check the prescribing information online-FDA-mandated labels now all follow the new structure.
Can I trust the data in the PLLR sections?
The data comes from human studies, animal research, and pregnancy registries. It’s reviewed by FDA scientists before approval. But it’s not perfect. Some drugs have limited data, especially for rare outcomes. The labels reflect what’s known-not what’s assumed. If a section says "data are limited," that’s a red flag to talk to your provider.
What if I took a drug before I knew I was pregnant?
The PLLR doesn’t include a separate section for accidental exposure because the risk doesn’t change based on intent. Instead, look at the Risk Summary and Clinical Considerations. If the drug has known risks, your provider may recommend monitoring (like extra ultrasounds). If the risk is low or unknown, they’ll likely reassure you. Don’t panic-most exposures don’t lead to problems.
Do PLLR labels apply to over-the-counter meds and supplements?
No. PLLR only applies to prescription drugs and biologics. OTC pain relievers, prenatal vitamins, herbal teas, and supplements are not covered. Always check with your provider before taking anything new-even if it’s "natural."
How do I find out if there’s a pregnancy registry for my medication?
Look in the Pregnancy section of the drug’s prescribing information. If a registry exists, it will be listed under "Data" with contact details. You can also search the FDA’s Pregnancy Registries website or ask your pharmacist. Enrolling helps build better safety data for future moms.




JUNE OHM
January 4, 2026 AT 01:09Philip Leth
January 5, 2026 AT 07:53Kerry Howarth
January 7, 2026 AT 02:05Tiffany Channell
January 9, 2026 AT 00:07Joy F
January 10, 2026 AT 04:53Haley Parizo
January 10, 2026 AT 06:11Ian Detrick
January 11, 2026 AT 01:51Angela Fisher
January 12, 2026 AT 00:56Neela Sharma
January 12, 2026 AT 11:04Shruti Badhwar
January 13, 2026 AT 06:14Brittany Wallace
January 14, 2026 AT 08:03Tru Vista
January 14, 2026 AT 15:07