When you see bright red blood in your stool, it’s terrifying. You might think it’s just hemorrhoids. But if you’re over 60 and the bleeding is sudden, heavy, and painless, it could be something more serious-like diverticula or angiodysplasia. These are two of the most common causes of lower gastrointestinal (GI) bleeding, and knowing the difference can save your life.
What Is Lower GI Bleeding?
Lower GI bleeding means blood is coming from somewhere in your colon, rectum, or anus-anywhere past the ligament of Treitz, which is deep inside your abdomen. It usually shows up as bright red or maroon blood in your stool, called hematochezia. Sometimes, it’s just a streak on the toilet paper. Other times, it’s a full-blown gush that turns the toilet water red. About 20 to 33% of all GI bleeds happen in the lower tract. Most patients are over 60. In the U.S., roughly 20 to 27 people out of every 100,000 get it each year. The good news? Most cases stop on their own. The bad news? If it doesn’t, and you don’t get checked quickly, you could end up in the hospital-or worse.Diverticula: The Silent Bleeder
Diverticula are small, balloon-like pouches that stick out from the wall of your colon. They’re super common-about half of all people over 60 have them. Most never cause problems. But in about 1 in 4 of those with diverticula, one of these pouches can start bleeding. Here’s how it happens: Blood vessels run close to the surface of the colon to feed the lining. When a diverticulum forms, it pushes these vessels outward. Over time, the vessel gets stretched thin and can rupture. There’s no inflammation, no pain, no warning. Just-bleeding. It’s often massive. Patients describe it as a sudden gush, sometimes enough to make them faint. But because there’s no cramping or fever, many people ignore it at first. That’s dangerous. Up to 50% of hospitalizations for lower GI bleeding are due to diverticula. The good part? About 80% of these bleeds stop on their own within 24 to 48 hours. But if it keeps going, you need help fast. Doctors will check your blood pressure, heart rate, and hemoglobin. If your hemoglobin is below 10 g/dL, you’re likely losing too much blood and may need a transfusion.Angiodysplasia: The Slow Leak
If diverticula are the loud, sudden bleeders, angiodysplasia is the quiet one. It’s also called vascular ectasia or arteriovenous malformation (AVM). Instead of pouches, you’ve got twisted, fragile blood vessels in the colon wall-usually on the right side, near the cecum. These vessels form because of aging. As you get older, the normal movement of your colon puts pressure on small arteries and veins. Over time, they stretch, thin out, and connect abnormally. Think of it like a garden hose that’s been kinked for years-eventually, it weakens and starts to leak. Unlike diverticula, angiodysplasia rarely causes big, dramatic bleeds. Instead, it drips slowly. You might not even notice blood in your stool. But over weeks or months, you start feeling tired. Your skin gets pale. You get short of breath climbing stairs. That’s iron deficiency anemia from chronic blood loss. About 3 to 6% of all lower GI bleeds come from angiodysplasia. But in people over 70, it’s the second most common cause after diverticula. And here’s the twist: if you have aortic stenosis (a narrowed heart valve), your risk goes up. The turbulent blood flow destroys a clotting protein called von Willebrand factor, making you bleed easier.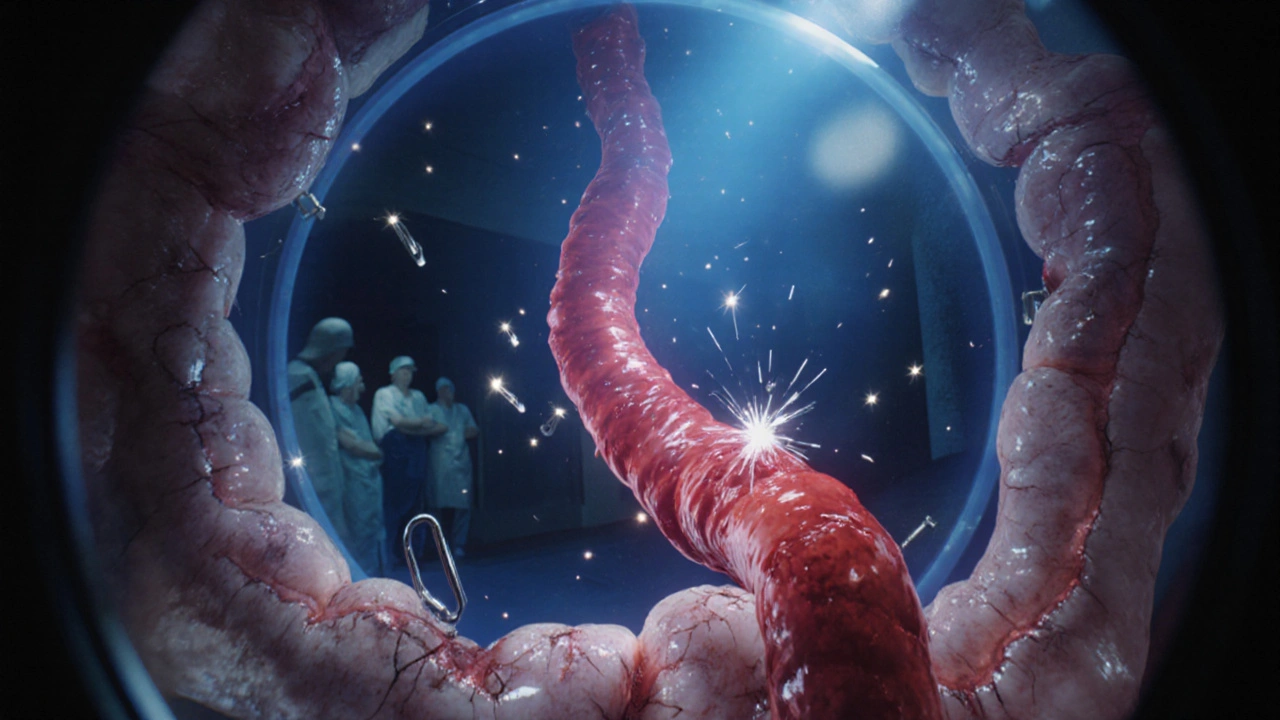
How Do Doctors Find the Source?
The first thing any ER doctor does when you show up with GI bleeding is stabilize you. They’ll give you IV fluids. They’ll check your vitals. If you’re pale, dizzy, or your heart is racing, they’ll order blood tests and prepare for a transfusion. Then comes the key test: colonoscopy. It’s the gold standard. Done within 24 hours of admission, it finds the source in over 80% of cases and can even treat it at the same time. Studies show patients who get colonoscopy within a day have 26% lower death rates than those who wait. But here’s the catch: if you’re bleeding heavily, your colon is full of blood. That makes it hard to see. Doctors use a trick-they give you IV fluids and a drug called erythromycin. It speeds up gut movement, helping clear the blood so the camera can get a clear view. If colonoscopy doesn’t find anything, you’ve got what’s called “obscure” GI bleeding. That’s when the bleed is coming from deeper in the small intestine. That’s where capsule endoscopy comes in. You swallow a pill-sized camera. It takes pictures as it travels through your gut. It finds the cause in about 62% of these cases. But there’s a risk. If you have a hidden narrowing in your intestine, the capsule can get stuck. That’s why some doctors wait until after a CT scan or device-assisted enteroscopy (a longer, more precise scope) if they suspect a stricture. CT angiography is another powerful tool. It can spot active bleeding as slow as 0.5 mL per minute. That’s useful if you’re too unstable for colonoscopy or if the bleed is intermittent. It’s fast, non-invasive, and highly accurate-85% sensitivity.Treatment: What Happens Next?
For diverticula bleeding, most cases don’t need surgery. If you’re stable, doctors will monitor you. If the bleeding continues, they’ll go back in with a colonoscope. They’ll inject epinephrine to shrink the blood vessels and use heat or clips to seal the spot. Success rate? 85 to 90%. But here’s the catch: 20 to 30% of people bleed again within a year. Angiodysplasia is trickier. The go-to treatment is argon plasma coagulation (APC). It’s like using a controlled electric spark to burn the abnormal vessels shut. It works immediately in 80 to 90% of cases. But because the vessels keep forming over time, 20 to 40% of patients bleed again within a year or two. For recurrent angiodysplasia, doctors have two medical options. One is thalidomide-yes, the same drug once used for morning sickness. Taken daily at 100 mg, it reduces bleeding by 70% in clinical trials. The other is octreotide, a hormone injection given three times a day. It helps constrict blood vessels and cuts bleeding by about 60%. Surgery is a last resort. If the bleeding keeps coming from the same spot-like the cecum-doctors may remove that section of the colon. Right hemicolectomy is common for angiodysplasia. For diverticula, they’ll remove only the affected segment.What’s New in 2025?
Technology is changing how we spot and treat these bleeds. AI-powered colonoscopes now flag tiny vascular lesions that human eyes might miss. One 2022 study showed a 35% increase in angiodysplasia detection using AI. New endoscopic clips are also making a difference. A 2023 European trial found a new type of clip achieved 92% hemostasis in diverticular bleeding-better than heat or injections. And there’s hope on the horizon. The NIH is running a phase III trial (NCT04567891) comparing thalidomide to placebo for recurrent angiodysplasia. Results are expected in late 2024. If it works, this could become standard care.
What’s the Long-Term Outlook?
The good news? Most people survive. Five-year survival rates are 78% for diverticula and 82% for angiodysplasia. But survival isn’t about the bleed-it’s about your other health problems. Heart disease, kidney disease, diabetes-they’re what really affect your outcome. The real challenge is recurrence. With diverticula, you might have one big scare and never bleed again. With angiodysplasia, you might need repeated hospital visits for years. Patients on support forums say it takes an average of 18 months to get diagnosed-many have had three or more negative colonoscopies before finding the culprit. That’s why follow-up matters. If you’ve had one bleed, your doctor should monitor your iron levels. They might recommend repeat colonoscopies or even a capsule endoscopy if you’re still anemic.When to Worry
Not every spot of blood is an emergency. But if you’re over 60 and you see:- Bright red blood in large amounts
- Blood with no pain or itching
- Signs of anemia-fatigue, dizziness, shortness of breath
- History of heart valve disease or high blood pressure
What You Can Do
You can’t prevent diverticula. But you can reduce your risk of bleeding:- Keep your bowel movements regular. Eat fiber-oats, beans, vegetables.
- Stay hydrated. Dehydration makes stools harder and increases pressure in the colon.
- Avoid NSAIDs like ibuprofen or naproxen. They can irritate the gut lining.
- Manage your blood pressure and heart health. These affect blood vessel strength.
Can diverticula bleeding be prevented?
You can’t prevent diverticula from forming, but you can lower your risk of bleeding by eating a high-fiber diet, staying hydrated, and avoiding NSAIDs. Regular colonoscopies after age 50 help catch problems early.
Is angiodysplasia cancer?
No, angiodysplasia is not cancer. It’s a vascular abnormality-fragile blood vessels in the colon wall. But because it can cause chronic bleeding and anemia, it’s often mistaken for colorectal cancer. A biopsy during colonoscopy can confirm it’s not malignant.
Why does angiodysplasia happen more in older adults?
As we age, the walls of our blood vessels weaken. Constant movement in the colon puts pressure on small arteries and veins, causing them to stretch and form abnormal connections. Over 80% of cases occur in people over 65, with an average age of 72 at diagnosis.
Can a colonoscopy miss angiodysplasia?
Yes. Angiodysplasia lesions are small and can be hidden by blood or mucus. If bleeding is intermittent, the lesion may not be active during the exam. That’s why some patients need repeat colonoscopies or capsule endoscopy if symptoms persist.
Is thalidomide safe for treating angiodysplasia?
Thalidomide is used off-label for recurrent angiodysplasia and has shown good results in clinical trials, reducing bleeding by 70%. It’s taken daily at 100 mg. Side effects include drowsiness, nerve damage, and birth defects-so it’s only used in older adults who aren’t pregnant and under close supervision.
How long does recovery take after GI bleeding?
Recovery depends on the cause and how much blood you lost. Most people feel better within a week after a one-time bleed. But if you have chronic anemia from angiodysplasia, it can take months to rebuild iron stores with supplements or transfusions. Follow-up blood tests are essential.


Lauryn Smith
December 2, 2025 AT 11:54So many people brush off blood in their stool like it’s no big deal. I’m so glad this post laid it out so clearly. If you’re over 60 and see red, just go get checked. No excuses. Your gut isn’t lying.
Bonnie Youn
December 4, 2025 AT 00:03My aunt bled for months and thought it was hemorrhoids until she passed out in the bathroom. They found three angiodysplasia lesions in her cecum. She’s on thalidomide now and it’s been a game changer. No more transfusions. Doctors need to talk about this more.
Suzanne Mollaneda Padin
December 4, 2025 AT 13:46I work in a GI clinic and see this every week. The hardest part isn’t the diagnosis-it’s getting people to come in before they’re pale and dizzy. We have a handout we give out that says ‘Red blood isn’t normal. Ever.’ It’s simple. It works.
Erin Nemo
December 6, 2025 AT 08:49Colonoscopy before lunch. That’s what my dad did. They found a diverticulum, clamped it, and he was home by dinner. No big surgery. No horror story. Just good medicine.
ariel nicholas
December 6, 2025 AT 11:03Wait… so you’re telling me that after decades of eating fiber, drinking water, and avoiding NSAIDs, I’m still just a ticking time bomb because I’m old? That’s not medicine, that’s capitalism. They sell you a colonoscopy, then a capsule, then a surgery, then a pill-then they tell you it’s just aging. Pathetic.
Rachel Stanton
December 6, 2025 AT 16:46AI-assisted colonoscopy is a game-changer, but we still need better training for residents. I’ve seen cases where a lesion was right there-clear as day-but the trainee missed it because they were rushing. Tech helps, but human eyes still matter. Especially when the bleed is intermittent.
Edward Hyde
December 8, 2025 AT 13:26Thalidomide? For real? That drug nearly wiped out a generation of babies. Now we’re giving it to old folks like it’s aspirin? And you call this progress? I’d rather bleed than take a drug that could’ve killed my grandparents. This isn’t science-it’s desperation.
Charlotte Collins
December 10, 2025 AT 02:14Let’s be honest: most of these cases are misdiagnosed because doctors are overworked and underpaid. The ‘gold standard’ colonoscopy? It’s often rushed. The capsule endoscopy? Expensive. The CT angiography? Not covered by insurance unless you’re on the brink of death. This isn’t medicine-it’s a lottery.
Amber-Lynn Quinata
December 10, 2025 AT 04:15I’m sorry but if you’re over 60 and still eating fast food and skipping colonoscopies, you’re not a victim-you’re a choice. I’ve seen people cry because they didn’t want to ‘face it’ and now they’re in the ICU. Wake up. Your body is not a myth. Your denial is the real disease. 😔
Margaret Stearns
December 11, 2025 AT 07:01My dad had two bleeds in three years. They found the second one only because he got a capsule endoscopy after three negative colonoscopies. Don’t give up if the first test is clean. Keep pushing. Your life matters more than a doctor’s schedule.
amit kuamr
December 12, 2025 AT 04:48In India we dont have capsule endoscopy in small towns. If you bleed you go to the hospital and if they dont have money you go home. No one tells you about thalidomide. We just pray. But this post is good. Maybe one day we will have this knowledge too.