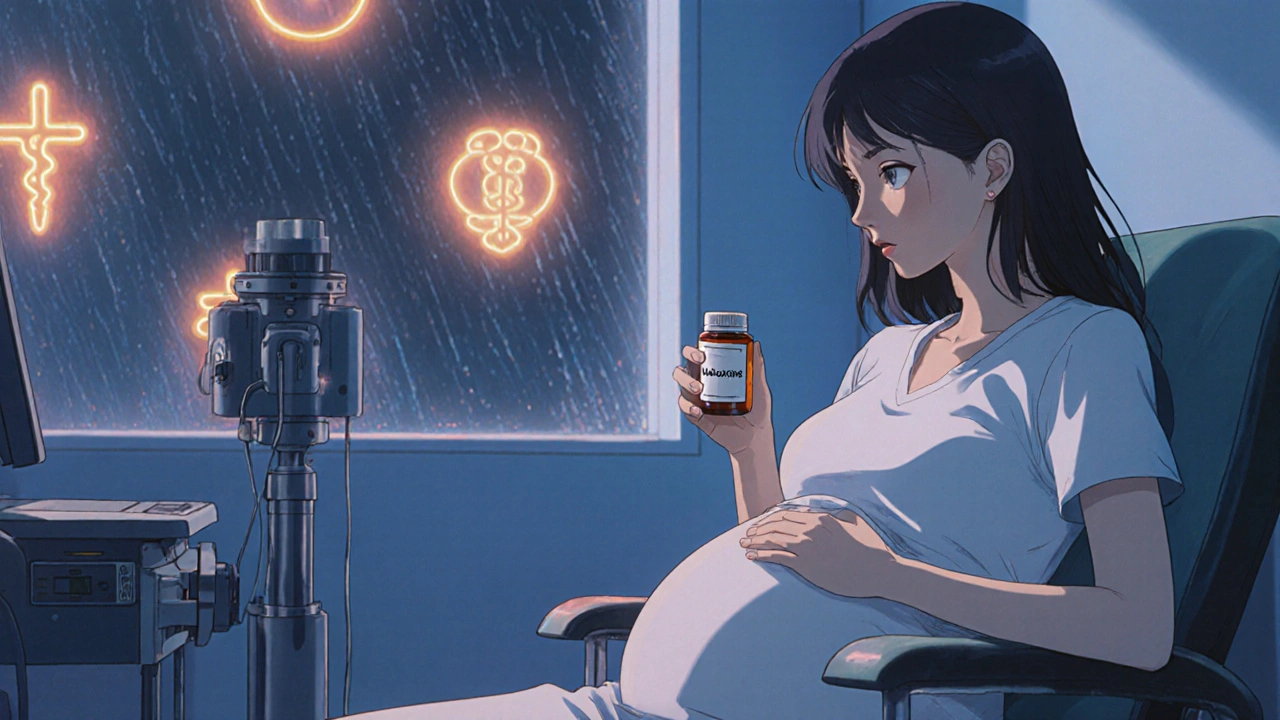
When you’re pregnant and struggling with opioid or alcohol use disorder, the fear of harming your baby can feel overwhelming. You want to get better-but you’re terrified that treatment might hurt your child more than the addiction itself. That’s where naltrexone comes in. It’s a medication used to block opioids and reduce alcohol cravings, but is it safe when you’re carrying a baby? The answer isn’t simple, and it’s not the same for everyone.
What Is Naltrexone?
Naltrexone is a medication approved by the FDA to treat opioid use disorder and alcohol use disorder. It works by attaching to opioid receptors in the brain and blocking the effects of drugs like heroin, oxycodone, or fentanyl. It doesn’t produce any high or euphoria. For people with alcohol dependence, it reduces the pleasurable effects of drinking, making it easier to cut back or stop.
It comes in two forms: a daily pill and a monthly injection (Vivitrol). The pill form is often used for alcohol dependence, while the injectable version is more common for opioid addiction. Neither form is addictive. Unlike methadone or buprenorphine, naltrexone doesn’t activate opioid receptors-it just blocks them.
Why Do Pregnant Women Consider Naltrexone?
Many pregnant women with opioid addiction face a hard choice: continue using drugs and risk miscarriage, preterm birth, or neonatal abstinence syndrome (NAS), or try to quit cold turkey-which can be dangerous and often leads to relapse. Medication-assisted treatment (MAT) has been the standard for years, but most MAT options like methadone and buprenorphine are opioids themselves. That’s why some women and doctors look at naltrexone as a non-opioid alternative.
For women who are already stable and have been opioid-free for at least 7-10 days, naltrexone can help prevent relapse during pregnancy. It’s especially appealing because it doesn’t cross the placenta in a way that causes dependence in the fetus. That means the baby won’t go through withdrawal at birth.
What Does the Research Say About Naltrexone and Pregnancy?
Studies on naltrexone in pregnancy are limited, but they’re growing. A 2021 review published in Obstetrics & Gynecology analyzed 12 clinical studies involving over 300 pregnant women who took naltrexone. The results showed no increase in major birth defects compared to the general population. The rate of congenital anomalies was around 2.3%, which is similar to the 2-3% baseline risk in any pregnancy.
Another study from 2023 followed 87 pregnancies where naltrexone was used. Only 11% of babies showed mild signs of NAS-far lower than the 50-80% rate seen with methadone or buprenorphine. Most of those cases didn’t require medication and resolved on their own within a few days.
There’s also no evidence that naltrexone causes low birth weight, stillbirth, or developmental delays. In fact, women on naltrexone were more likely to attend prenatal visits and stay off illicit drugs throughout pregnancy compared to those who tried to quit without medication.
When Is Naltrexone Not Recommended During Pregnancy?
Even though the data is reassuring, naltrexone isn’t for everyone. It should never be started while you’re still using opioids. If you’re actively using, naltrexone can trigger sudden, severe withdrawal-something that could cause uterine contractions and lead to preterm labor or fetal distress.
You also need to be completely opioid-free for at least 7 to 10 days before starting naltrexone. That’s not easy to do without support. Most women who start naltrexone during pregnancy have already been in detox or are in a structured treatment program with counseling.
Women with liver disease should avoid naltrexone. The medication is processed by the liver, and high doses can cause liver enzyme spikes. Routine blood tests are recommended during treatment.
And while the injectable form (Vivitrol) is often preferred for compliance, it’s not typically used in early pregnancy unless absolutely necessary. The long-acting nature means you can’t stop it quickly if side effects arise.
How Does Naltrexone Compare to Methadone and Buprenorphine?
For decades, methadone and buprenorphine have been the go-to treatments for opioid addiction in pregnancy. Both are considered safe and effective, and they’re backed by decades of research. But they come with a trade-off: the baby becomes dependent on them and may experience NAS after birth.
Naltrexone doesn’t cause fetal dependence. That’s its biggest advantage. But it’s harder to start. You need to be fully detoxed first, which many women aren’t ready for. Methadone and buprenorphine can be started immediately-even while you’re still using-making them more accessible.
Here’s a quick comparison:
| Feature | Naltrexone | Methadone | Buprenorphine |
|---|---|---|---|
| Does it cross placenta? | Yes, but doesn’t activate opioid receptors | Yes, causes fetal dependence | Yes, causes mild fetal dependence |
| Requires detox before starting? | Yes (7-10 days opioid-free) | No | No |
| Risk of neonatal abstinence syndrome (NAS) | Low (5-15%) | High (50-80%) | Moderate (30-50%) |
| Form available | Pill, monthly injection | Daily oral liquid | Daily sublingual tablet or film |
| Can be started in early pregnancy? | Only after detox | Yes | Yes |
For women who have already stabilized on methadone or buprenorphine, switching to naltrexone during pregnancy is possible but risky. Most providers don’t recommend it unless there’s a strong reason-like a history of misuse of the opioid-based meds.
What Are the Side Effects of Naltrexone in Pregnancy?
Most women tolerate naltrexone well. Common side effects include nausea, headaches, dizziness, and fatigue. These usually fade after the first few weeks. Some women report trouble sleeping or mild anxiety.
There’s no evidence that naltrexone causes birth defects, but it’s still a relatively new option in pregnancy. The FDA classifies it as Category C-meaning animal studies showed some risk, but human data is limited. That doesn’t mean it’s unsafe. It just means we don’t have massive long-term studies yet.
One thing to watch for: naltrexone can make you more sensitive to opioids after pregnancy. If you relapse after giving birth, even a small dose could be dangerous because your tolerance has dropped. That’s why ongoing counseling and support are critical.
What Should You Do If You’re Pregnant and Taking Naltrexone?
If you’re already on naltrexone and just found out you’re pregnant, don’t stop it suddenly. Talk to your provider right away. Stopping abruptly could trigger cravings and increase your risk of relapse, which is far more dangerous to your baby than continuing the medication.
Your doctor will likely:
- Check your liver function with blood tests
- Confirm you’re still opioid-free
- Adjust your dose if needed (usually no change)
- Refer you to a prenatal addiction specialist
- Coordinate with your counselor or therapist
Most women continue naltrexone through pregnancy without issues. The key is staying connected to care. Regular ultrasounds, growth scans, and mental health support make a huge difference in outcomes.

Can You Breastfeed While Taking Naltrexone?
Yes. Naltrexone passes into breast milk in very small amounts-less than 1% of the maternal dose. Studies show no adverse effects in nursing infants. The American Academy of Pediatrics considers it compatible with breastfeeding.
If you’re on the monthly injection, you can still breastfeed. There’s no need to pump and dump. The low levels in milk are not enough to affect the baby.
Still, watch your baby for unusual sleepiness, poor feeding, or irritability. These are rare but worth reporting to your pediatrician.
Final Thoughts: Is Naltrexone Safe During Pregnancy?
There’s no perfect answer. But based on current evidence, naltrexone appears to be a safe and viable option for pregnant women who are opioid-free and need help staying that way. It’s not a first-line treatment like buprenorphine-but for some women, it’s the best choice.
If you’re considering naltrexone during pregnancy, work with a provider who specializes in addiction medicine and prenatal care. Don’t make this decision alone. You’re not choosing between addiction and medication-you’re choosing between uncontrolled use and a safer path for you and your baby.
Recovery during pregnancy is hard. But with the right support, it’s possible. And naltrexone might just be the tool that helps you get there without putting your baby at risk.
Can naltrexone cause miscarriage during pregnancy?
There is no evidence that naltrexone increases the risk of miscarriage. Studies tracking over 300 pregnancies found no higher rate of pregnancy loss compared to the general population. The main risk comes from untreated opioid use-not from naltrexone itself.
Is naltrexone safe in the first trimester?
Yes, naltrexone can be used safely in the first trimester, as long as you’ve been opioid-free for at least 7-10 days before starting. The critical period for organ development ends by week 10, and studies show no increase in birth defects when naltrexone is used after that point. Starting earlier is possible with medical supervision.
Can I switch from methadone to naltrexone while pregnant?
Switching from methadone to naltrexone during pregnancy is possible but risky. You must stop methadone completely and wait 7-10 days to avoid severe withdrawal. This process can trigger stress, contractions, or preterm labor. Most providers recommend staying on methadone or buprenorphine unless there’s a strong medical reason to switch.
Does naltrexone affect fetal development or IQ?
No studies have shown that naltrexone affects a baby’s brain development or lowers IQ. Children exposed to naltrexone in utero have shown normal cognitive and motor development through age 2 in follow-up studies. The bigger risk to development comes from ongoing drug use, poor nutrition, or lack of prenatal care.
What if I relapse while on naltrexone during pregnancy?
If you relapse while on naltrexone, the medication will block the effects of opioids, so you won’t feel the high. But you’re still putting yourself and your baby at risk through unsafe use, overdose, or exposure to contaminated drugs. Relapse is common in addiction recovery-reach out to your provider immediately. They can help you adjust your treatment plan without judgment.
Next Steps If You’re Considering Naltrexone
Start by talking to your OB-GYN or a maternal-fetal medicine specialist. Ask if they work with addiction specialists. If not, contact a local substance use treatment center that offers prenatal care. The Substance Abuse and Mental Health Services Administration (SAMHSA) has a free helpline: 1-800-662-HELP (4357). They can connect you to providers who understand both pregnancy and addiction.
Don’t wait until your next appointment. If you’re using opioids or alcohol and pregnant, time matters. Every day of sobriety improves your baby’s chances. Naltrexone isn’t a magic fix-but for many women, it’s the bridge to a healthier pregnancy and a brighter future for their child.



Pooja Surnar
October 30, 2025 AT 04:53Mark Gallagher
October 30, 2025 AT 19:01Wendy Chiridza
October 31, 2025 AT 16:53Gerald Nauschnegg
November 2, 2025 AT 05:15Palanivelu Sivanathan
November 3, 2025 AT 08:08Joanne Rencher
November 3, 2025 AT 18:09Cristy Magdalena
November 4, 2025 AT 16:33Casey Lyn Keller
November 6, 2025 AT 01:41Jessica Ainscough
November 6, 2025 AT 02:12Sara Larson
November 8, 2025 AT 01:49Mindy Bilotta
November 8, 2025 AT 02:32Brian Perry
November 8, 2025 AT 22:53