Most people don’t realize their drinking is quietly damaging their liver until it’s too late. You might feel fine. You might not even consider yourself a heavy drinker. But if you’re having a few drinks most days, your liver could already be in trouble. Alcohol-associated liver disease (ALD) doesn’t announce itself with a siren. It creeps in silently, stage by stage, turning a healthy organ into scar tissue over years-or sometimes just months. The good news? The early stages can be reversed. The bad news? Once cirrhosis sets in, the damage is mostly permanent. Knowing the stages isn’t just medical trivia-it could save your life.
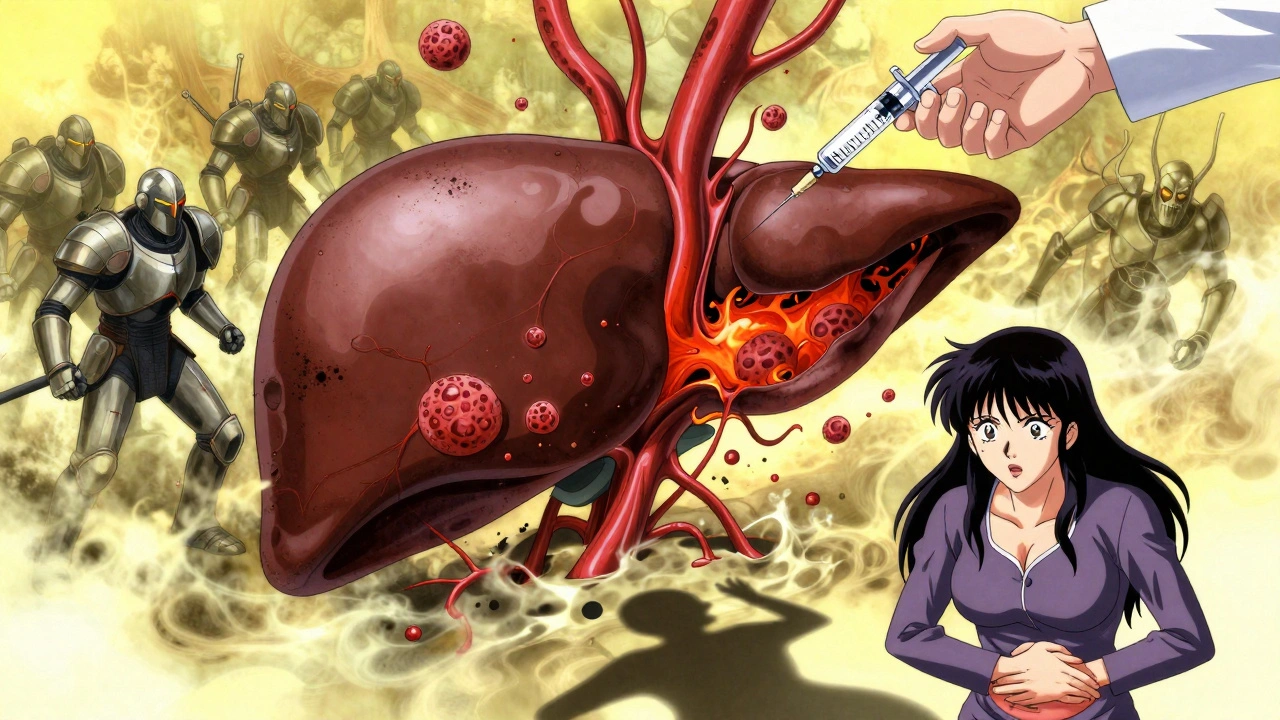
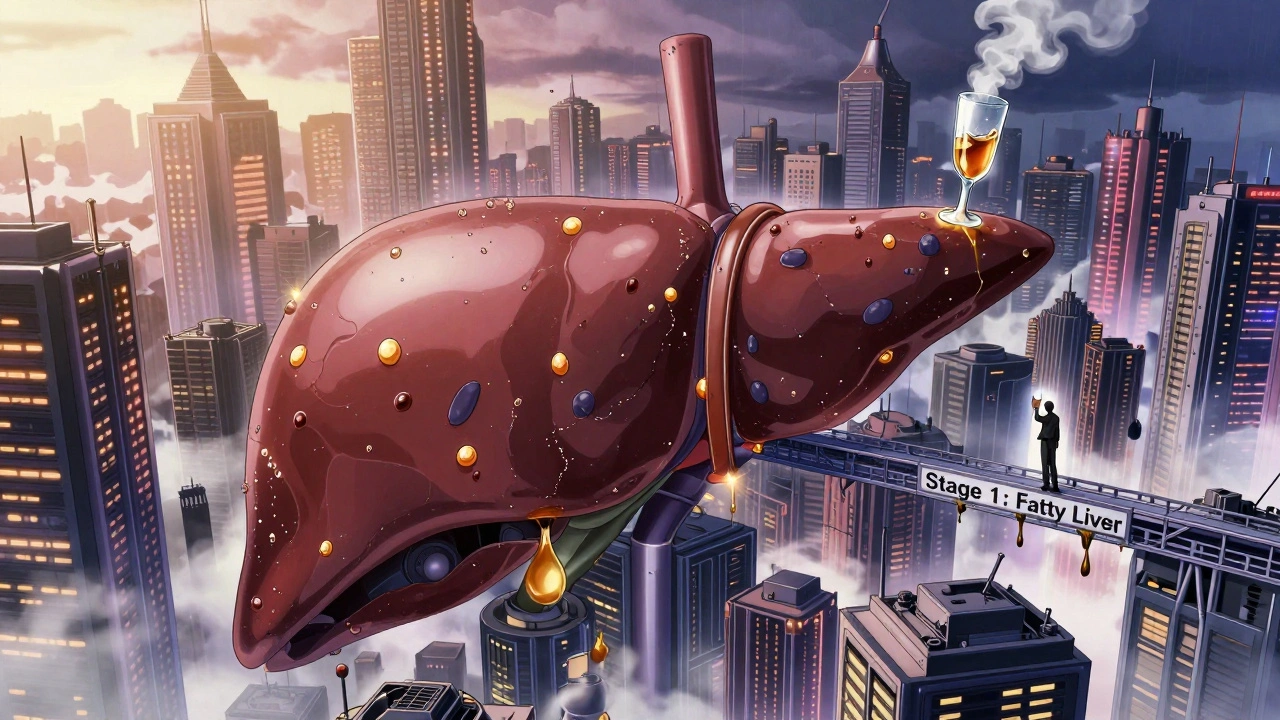
Stage 1: Fatty Liver (Alcoholic Steatosis)
This is where it starts. Almost everyone who drinks heavily-more than 3-4 standard drinks a day-will develop fatty liver. That’s right: up to 90% of people who drink this much will have fat building up in their liver cells. It’s not a diagnosis you’ll feel. Most people have no symptoms at all. No pain. No jaundice. No fatigue. You might just think you’re tired from work or stressed out.
What’s happening inside? Alcohol breaks down into toxins that overwhelm your liver’s ability to process fat. Instead of burning it off, your liver stores it. When fat makes up more than 5-10% of your liver’s weight, it’s classified as steatosis. Blood tests might show slightly elevated liver enzymes-AST and ALT-with AST usually higher than ALT, often in a 2:1 ratio. That’s a classic red flag doctors look for.
Here’s the critical part: this stage is 100% reversible. If you stop drinking for just 4 to 6 weeks, your liver can clear out the fat. A 2017 clinical trial showed 85% of people who quit alcohol completely saw their fatty liver vanish. No pills. No surgery. Just abstinence. The British Liver Trust calls this the easiest stage to fix-and the most ignored. People get diagnosed, hear "it’s just fatty liver," and think, "I’m fine." They’re not. This is your body screaming for a change.
Stage 2: Alcoholic Hepatitis (Alcohol-Associated Hepatitis)
Now things get serious. If you keep drinking after fatty liver, about one in three people will develop alcoholic hepatitis. This isn’t just fat anymore. Now your liver is inflamed. Liver cells are dying. Immune cells swarm in, causing swelling and damage. Symptoms start to appear: yellow skin and eyes (jaundice), nausea, fever, abdominal pain, and extreme fatigue. Some people feel like they have the flu-only it doesn’t go away.
Doctors use the Maddrey Discriminant Function (mDF) score to measure severity. If your score is 32 or higher, you have severe alcoholic hepatitis. That means a 30-40% chance of dying within 30 days if you don’t get treatment. Even mild cases carry a 4-10% death risk. And here’s the scary part: half of all people with severe alcoholic hepatitis have never been told they had liver problems before. The disease hides until it’s advanced.
Treatment isn’t simple. Stopping alcohol is non-negotiable. But if you’re in the severe range, you’ll likely need steroids like prednisolone. The STOPAH trial showed steroids cut 28-day death rates from 20% to under 18%. But here’s the catch: only about 40% of patients respond. For those who don’t, the options are limited. Some need intensive care. Others need a liver transplant.
Women are at higher risk. They develop alcoholic hepatitis after drinking less than men-sometimes half the amount. Why? Their bodies process alcohol differently. They have less of the enzyme that breaks it down in the stomach, so more alcohol reaches the liver. Genetics matter too. If you carry certain gene variants like PNPLA3, your risk jumps even if you drink moderately.
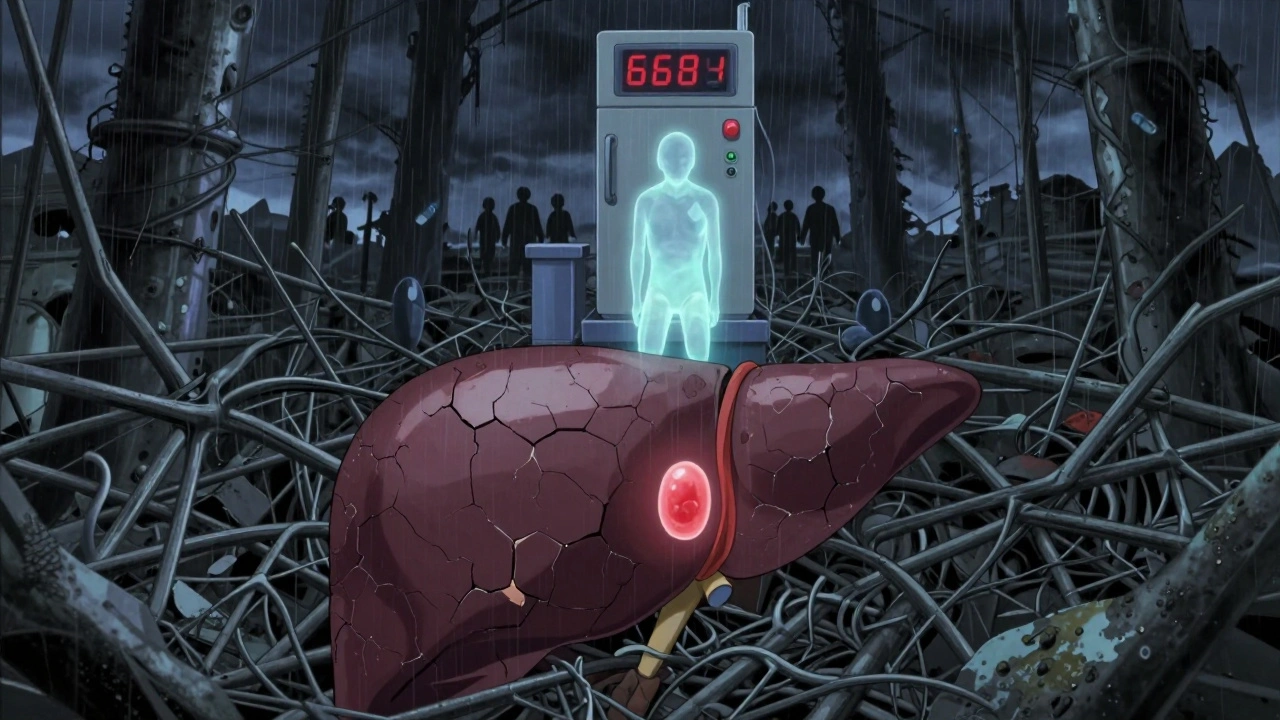
Stage 3: Cirrhosis (Alcohol-Associated Cirrhosis)
Cirrhosis is the point of no return. Not because it’s untreatable-but because the damage is structural. Your liver, once soft and spongy, is now a web of scar tissue. More than 75% of healthy liver structure is gone. The liver can still function for a while-that’s called compensated cirrhosis. But it’s barely holding on.
At this stage, your liver can’t filter toxins well. It can’t make proteins. It can’t regulate blood flow. Complications start piling up: fluid builds up in your belly (ascites), veins in your esophagus swell and can burst (varices), you get confused or drowsy from toxins in your blood (hepatic encephalopathy), and your kidneys start failing (hepatorenal syndrome). One in three people with cirrhosis will develop liver cancer.
Once you’re here, abstinence is your last best shot. Studies show that if you stop drinking completely after cirrhosis is diagnosed, your 5-year survival rate jumps from 30% to 70-90%. If you keep drinking? Median survival drops to just 1.8 years. That’s not a guess. That’s from long-term data tracked by the NHS.
Liver transplantation is the only cure. But most centers require six months of verified sobriety before putting you on the list. Why? Because if you go back to drinking after the transplant, your new liver will fail again. The success rate is good-70-75% survive five years post-transplant-but the waiting list is long. And not everyone qualifies.
There’s new hope. Fecal microbiota transplants (FMT) showed a 40% improvement in 90-day survival in a 2022 Lancet trial. New drugs targeting inflammation are in phase 2 trials. But none of this matters if you don’t stop drinking.
Who’s at Risk? It’s Not Just Heavy Drinkers
Many assume only binge drinkers or people with alcohol use disorder get ALD. That’s a myth. A 2023 study in JAMA Internal Medicine found hospitalizations for ALD rose 65% among 25-34-year-olds between 2010 and 2020-especially in women. Many of these people weren’t "alcoholics." They were having two drinks a night, five nights a week. That’s 70 grams of alcohol daily-enough to cause liver damage over time.
Women are more vulnerable. So are people with obesity, diabetes, or hepatitis C. Even moderate drinking speeds up liver scarring in people with fatty liver disease from other causes. If you have NAFLD and drink 20-40 grams of alcohol a day, your fibrosis progresses three times faster than if you abstain.
Genetics play a huge role. Two gene variants-PNPLA3 and TM6SF2-make your liver more sensitive to alcohol. You could be someone who drinks lightly and still develops cirrhosis. Or you could be a heavy drinker who never does. It’s not about willpower. It’s biology.
Diagnosis: No Symptoms Doesn’t Mean No Damage
Most people with fatty liver or even early alcoholic hepatitis have no symptoms. That’s why blood tests and imaging matter. Routine liver enzyme tests (ALT, AST, GGT) are the first clue. An AST-to-ALT ratio above 2 is a strong indicator of alcohol-related damage.
Today, you don’t always need a liver biopsy. FibroScan, a painless ultrasound-based test, can detect fibrosis with 85-90% accuracy. It’s quick, non-invasive, and increasingly standard in clinics. If your FibroScan shows F2 or higher fibrosis, you’re already in danger zone.
Doctors also use scoring systems like the Glasgow Alcoholic Hepatitis Score (GAHS) and Lille Model to predict outcomes. A GAHS score of 9 or higher means over 50% chance of dying within six months without a transplant.
What Happens If You Keep Drinking?
Progression isn’t guaranteed-but it’s likely. One study showed that 10-20% of heavy drinkers develop cirrhosis. But if you keep drinking after fatty liver, your chances of reaching cirrhosis jump dramatically. And once you’re in cirrhosis, continuing to drink slashes your life expectancy in half.
Real stories from patient forums tell the same tale: "I was told I had fatty liver at 38. I didn’t stop. By 41, I was hospitalized for ascites. By 43, I was on the transplant list." Or: "I drank two glasses of wine every night for 15 years. My doctor said it was fine. Then I got jaundiced. That’s when they found cirrhosis."
Stigma is real. Many patients say doctors blamed them instead of helping. One in two people with ALD report feeling judged by healthcare workers. That delays care. It kills.
Recovery Is Possible-But Only If You Act
There’s no magic pill. No supplement. No detox tea. The only proven treatment for every stage of ALD is stopping alcohol completely. And the earlier you do it, the better your odds.
If you’re in stage one-fatty liver-quit now. In six weeks, your liver can heal. You might even feel better than you have in years.
If you’re in stage two-alcoholic hepatitis-quit immediately. You might need steroids. You might need hospitalization. But if you stop drinking, you can survive. Many do.
If you’re in stage three-cirrhosis-quit anyway. Your survival time could go from 1.8 years to over 12. You might get on a transplant list. You might live to see your kids graduate. You might not die of liver failure.
Support exists. Integrated care-where hepatologists work with addiction specialists-doubles your chance of staying sober for a year. That’s not a theory. It’s data from 2023 studies.
Your liver doesn’t care how much you drink. It doesn’t care if you’re "functional." It only responds to what you give it. And it’s a forgiving organ-if you give it a chance.
Can you reverse alcoholic liver disease?
Yes-up to a point. Fatty liver can be fully reversed with 4-6 weeks of complete alcohol abstinence. Alcoholic hepatitis can be reversed if caught early and you stop drinking immediately. Cirrhosis cannot be reversed, but stopping alcohol can stop further damage and significantly improve survival. The earlier you quit, the better your chances.
How much alcohol causes liver damage?
As little as 3-4 standard drinks a day over time can lead to fatty liver. For women, damage can occur with even less-sometimes 2 drinks daily. Heavy drinking is defined as more than 40-80 grams of pure alcohol daily (about 3-6 drinks). But there’s no safe threshold. Genetics, gender, and other health conditions all affect how your liver responds.
Do you have to be an alcoholic to get alcoholic liver disease?
No. The term "alcoholic" is misleading. Many people with ALD don’t have alcohol use disorder. They’re regular drinkers-two to four drinks a night-who didn’t realize the long-term impact. The American Association for the Study of Liver Diseases now uses "alcohol-associated" to reflect this. It’s about the amount and duration of alcohol, not addiction.
Can a liver transplant cure alcoholic liver disease?
A transplant can replace a failed liver, but it’s not a cure for the underlying cause. Most transplant centers require at least six months of verified sobriety before listing. If you return to drinking after transplant, your new liver will likely fail again. Transplant success depends on lifelong abstinence.
What are the early warning signs of liver damage from alcohol?
Early signs are often invisible. But if you notice unexplained fatigue, nausea, loss of appetite, or mild abdominal discomfort, it could be a signal. More obvious signs include yellowing skin or eyes (jaundice), swelling in the belly or legs, confusion, or dark urine. Blood tests showing elevated AST and ALT, especially with AST higher than ALT, are key early indicators.
What Comes Next?
If you’ve read this far, you’re probably wondering what to do next. If you’re drinking regularly, get your liver checked. Ask for a FibroScan or liver enzyme panel. Don’t wait for symptoms. If you’re diagnosed with fatty liver, don’t brush it off. That’s your wake-up call. If you’re struggling to quit, reach out. Support groups, counseling, and medication-assisted treatment can help. Your liver doesn’t need perfection-it just needs you to stop.






Jessica Baydowicz
December 3, 2025 AT 22:12Yo, I just got my FibroScan results and it showed F2 fibrosis 😳 I thought my 2 glasses of wine nightly were "fine"-turns out, my liver’s screaming for a timeout. Thanks for this post, I’m quitting cold turkey starting tomorrow. No more excuses.
Jordan Wall
December 5, 2025 AT 01:29Actually, the AST:ALT >2 ratio is a classic marker, but it's not universally reliable-especially in obese populations where NAFLD can skew the ratio. Also, the PNPLA3 rs738409 variant has a 3.5x increased risk for progression, per J Hepatol 2021. And let’s not forget the gut-liver axis-FMT is promising but still experimental. You’re oversimplifying a complex pathophysiology.
val kendra
December 6, 2025 AT 02:51I was diagnosed with fatty liver at 32. Dr said "just cut back" so I went from 6 drinks/week to 4. Big mistake. Two years later, I had hepatitis. Stopped drinking. Went to therapy. Did the 6-month sobriety thing for transplant eval. Now I’m 38, liver stable, and I’ve never felt lighter. It’s not about willpower. It’s about listening. Your liver doesn’t lie. And it doesn’t care if you’re "functional." It just wants you to stop.
jagdish kumar
December 6, 2025 AT 04:15Life is a series of choices… but the liver? The liver remembers every sip. 🌱
Carolyn Ford
December 6, 2025 AT 17:57Everyone’s so quick to blame alcohol-but what about the sugar? The processed foods? The stress? This post is pure fearmongering. I’ve seen people with cirrhosis who never drank a drop. This is just another way to shame people into conformity.
Elizabeth Crutchfield
December 8, 2025 AT 02:53my doctor told me my liver enzymes were "a little high" but didn’t say why. I thought it was from working out. Turns out it was 2 glasses of wine every night for 7 years. I cried in the parking lot. I’m 34. I didn’t think I was at risk. This post scared me into changing. Thank you.
Alex Piddington
December 9, 2025 AT 19:28Great breakdown. I work in a clinic and see this every week. People come in with AST 180, ALT 90, GGT 400, and say "I only drink on weekends." They don’t realize "weekend drinking" is 20+ drinks in 48 hours. That’s not social-it’s toxic. We need better screening protocols.
Shofner Lehto
December 10, 2025 AT 07:41My dad had alcoholic hepatitis at 52. He quit cold turkey, got on prednisolone, and now he’s 60 and hiking in the Rockies. He says the hardest part wasn’t quitting alcohol-it was facing how much he’d ignored his body for decades. If you’re reading this and you drink regularly, ask yourself: are you protecting your health-or just avoiding the truth?
Michael Feldstein
December 11, 2025 AT 15:43What’s the data on people who quit after cirrhosis diagnosis but don’t get a transplant? Do they stabilize? Or does it just slow the decline?
val kendra
December 12, 2025 AT 12:42Stabilization is possible. In compensated cirrhosis, abstinence leads to fibrosis regression in 30-40% of cases over 5 years, per NEJM 2020. It doesn’t reverse the scar tissue, but it stops the engine of inflammation. The liver rebuilds functional tissue around the scars. Survival rates jump because complications like ascites and varices don’t develop as fast. You’re not cured-but you’re no longer on a one-way train to death.
George Graham
December 14, 2025 AT 11:12I used to work with a guy who drank 6 beers a night. Said he was "fine." Got diagnosed with cirrhosis at 45. He started attending AA meetings, got a liver transplant, and now volunteers at the clinic. He told me: "I didn’t lose my liver. I lost my denial. That’s what saved me." You don’t need to be an alcoholic to need help. You just need to be ready to listen.
michael booth
December 14, 2025 AT 17:07It is imperative to underscore that the term "alcoholic" carries significant stigma and impedes early intervention. The American Association for the Study of Liver Diseases has rightly transitioned to "alcohol-associated liver disease" to promote a more compassionate, evidence-based clinical approach. This linguistic shift reflects a paradigm change in public health.
Libby Rees
December 16, 2025 AT 12:59I’m a nurse. I’ve seen too many people wait until they’re in the ICU before they admit their drinking is a problem. The ones who survive? They’re the ones who quit before symptoms hit. This post isn’t scary. It’s a gift.
Isabelle Bujold
December 18, 2025 AT 04:26Let me tell you about my cousin. She was 31, worked in marketing, drank one glass of wine with dinner every night. No binges. No blackout nights. Just… routine. Got a routine blood test. AST 140, ALT 70. FibroScan showed F3 fibrosis. She cried for three days. Then she quit. No rehab. No group. Just stopped. Two years later, her liver enzymes are normal. Her FibroScan is F0. She says she didn’t lose wine-she gained her future. The scary part? She’s not unusual. Thousands are doing this right now. And no one talks about it. We need more stories like this. Not fear. Not shame. Just truth.