More than 1 in 4 adults worldwide have fat building up in their liver - not from drinking alcohol, but from how they eat, move, and manage their metabolism. This isn’t just a minor issue. It’s now called MASLD - Metabolic Dysfunction-Associated Steatotic Liver Disease - and it’s becoming the leading cause of liver problems in the U.S. and Europe. The good news? You can reverse it. The better news? Weight loss and newer medications like semaglutide and liraglutide aren’t just helping with weight - they’re healing the liver.
What Exactly Is MASLD?
MASLD used to be called NAFLD - non-alcoholic fatty liver disease. But that name was misleading. It suggested you just had fat in your liver and nothing else was wrong. That’s not true. MASLD means your body’s metabolism is out of sync. You likely have insulin resistance, high blood sugar, extra belly fat, or high triglycerides. The liver gets overwhelmed. It starts storing fat instead of burning it.
Doctors now diagnose MASLD by what’s present, not what’s missing. If you have more than 5% fat in your liver and at least one metabolic issue - like being overweight, having type 2 diabetes, or high blood pressure - you have MASLD. No need to rule out other causes. The metabolic dysfunction is the cause.
For many, it stays harmless. But about 1 in 5 people with MASLD develop MASH - the more serious form where inflammation and scarring start. Left unchecked, MASH can lead to cirrhosis or liver cancer. The good news? This progression isn’t inevitable. It’s often reversible - especially with early action.
Why Weight Loss Is the Most Powerful Tool
There’s no magic pill for MASLD. But there is a proven, powerful fix: losing weight. And it’s not about looking lean. It’s about healing your liver.
Studies show that losing just 5% to 7% of your body weight reduces liver fat by up to 30%. That’s measurable on scans. But if you want to reduce inflammation and even reverse early scarring, you need to hit 10% or more. People who lose 10% or more have a 45% chance of completely clearing MASH - the inflammatory stage.
Here’s how it works inside your body:
- When fat cells are swollen from excess calories, they leak free fatty acids into your bloodstream - about 59% of the fat that ends up in your liver comes from this source.
- Insulin resistance makes your liver produce even more fat from sugar and carbs - another 26% of the problem.
- When you lose weight, your fat cells shrink. That cuts the fatty acid flood to your liver by 30-40%.
- Your liver also starts burning fat better and stops making so much new fat from carbs.
The Look AHEAD trial showed that people who lost 10% of their weight through diet and exercise cut their risk of developing MASH by 90%. That’s not a small effect. That’s life-changing.
But losing 10% isn’t easy. Most people regain the weight within two years. That’s why weight loss needs structure - not just willpower.
GLP-1 Agonists: The New Game-Changer
For many, diet and exercise alone aren’t enough. That’s where GLP-1 receptor agonists come in. These are injectable medications originally designed for type 2 diabetes - but their weight-loss effects changed everything.
Drugs like semaglutide (Wegovy®, Ozempic®) and liraglutide (Saxenda®) work by mimicking a natural hormone your gut releases after eating. It tells your brain you’re full, slows digestion, and improves how your body uses insulin.
The results are dramatic:
- In the STEP-1 trial, people using semaglutide 2.4 mg lost an average of 15.1% of their body weight.
- In those with MASLD, liver fat dropped by 55% - measured by MRI scans.
- Liraglutide helped 39% of patients clear MASH, compared to just 17% on placebo.
- Even the lower dose of semaglutide (1.0 mg, used for diabetes) led to 52% MASH resolution in the REGENERATE trial.
These drugs don’t just help you lose weight - they directly improve liver health. They reduce fat production in the liver by 20-25%. They lower inflammation by blocking key signaling pathways. And they make fat tissue more sensitive to insulin, cutting the flood of fatty acids that feed liver damage.
For people with type 2 diabetes and MASLD, GLP-1 drugs are now the first-line treatment after lifestyle changes. They tackle both problems at once.

Combining Weight Loss and GLP-1 Drugs Works Best
Using GLP-1 drugs without changing your diet? You’ll lose weight, but not as much. And the liver won’t heal as well.
Using diet and exercise without medication? Hard to reach and keep the 10% loss needed for real healing.
The best results come from combining both. A study from the MASLD Patient Registry found that people who got GLP-1 drugs and regular dietitian support had a 65% adherence rate after 12 months. Those on medication alone? Only 42% stuck with it.
Why? Because GLP-1 drugs make it easier to eat less. But if you’re still eating ultra-processed foods, drinking sugary drinks, or skipping movement, the liver won’t fully recover. The medication removes the hunger, but you still need to choose the right foods.
Experts recommend a Mediterranean-style diet - rich in vegetables, olive oil, nuts, fish, and whole grains. Cut back on fructose (found in soda, candy, and sweetened juices). Aim for 150-300 minutes of moderate exercise per week - walking, cycling, swimming. And pair that with your GLP-1 medication.
Side Effects and Real-World Challenges
GLP-1 drugs aren’t perfect. Nausea is the most common side effect - about 76% of users report it. For most, it’s mild and fades after a few weeks. But 32% of people quit within six months because it’s too uncomfortable.
Some people get vomiting, diarrhea, or constipation. Rarely, there’s risk of pancreatitis or gallbladder issues. But these are uncommon.
Cost is another barrier. In the U.S., semaglutide costs around $1,350 a month. Liraglutide is similar. Insurance coverage is improving - Medicare now covers about two-thirds of users for obesity - but many still pay out of pocket.
And here’s the big catch: if you stop the drug, you’ll likely regain weight - and liver fat will creep back. These aren’t cure pills. They’re tools for long-term management. That’s why combining them with lasting lifestyle changes is so critical.
What’s Next? New Treatments and Better Tools
The field is moving fast. In March 2024, the FDA is expected to approve resmetirom - the first drug specifically for MASH. It targets liver metabolism directly and may work well alongside GLP-1 drugs.
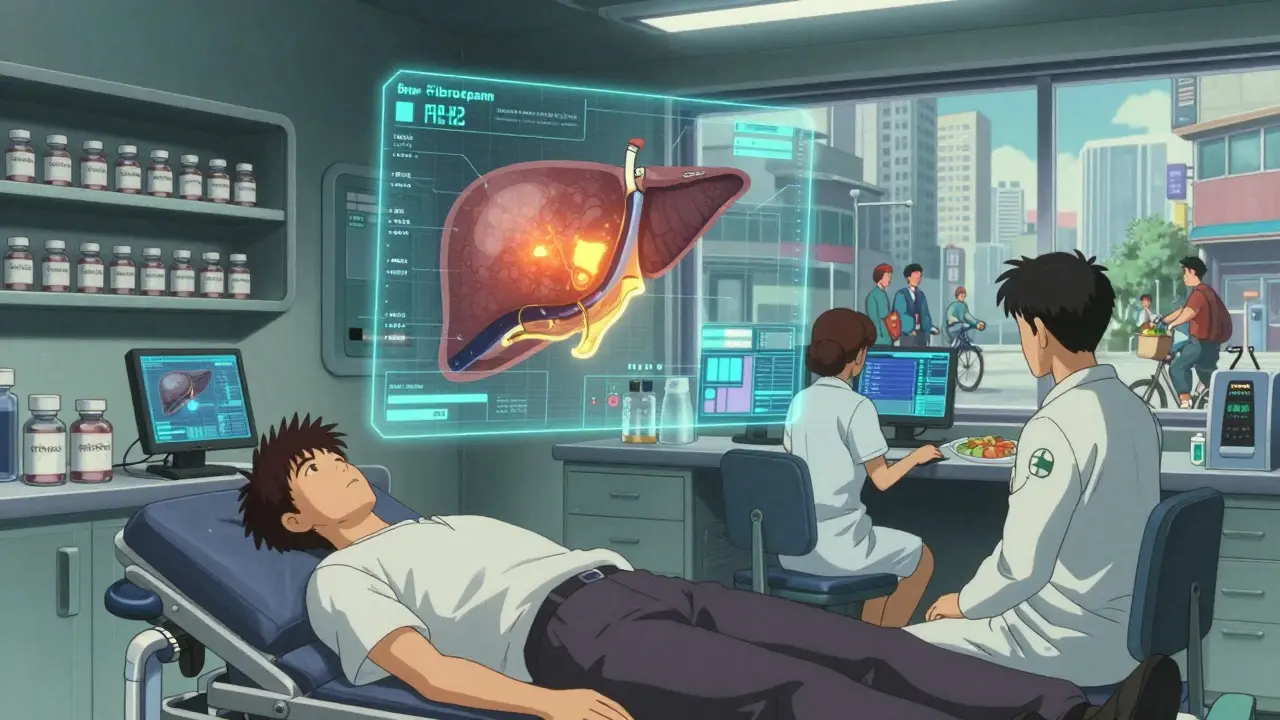
Doctors now use non-invasive tools to track progress: FibroScan measures liver stiffness (scarring) and fat content. MRI-PDFF gives precise fat percentages. Blood tests like FIB-4 help estimate fibrosis risk without a biopsy.
More clinics are opening - 72% of U.S. academic hospitals now have MASLD programs. But in rural areas, access is still limited. And not every doctor knows how to manage these drugs properly.
The big picture? MASLD is no longer just a liver issue. It’s a metabolic disorder that affects your heart, kidneys, and lifespan. The same lifestyle changes that heal your liver also lower your risk of heart attack and stroke. GLP-1 drugs, when used right, do the same.
What Should You Do Now?
If you’ve been told you have fatty liver, don’t wait. Start with these steps:
- Get a FibroScan or MRI-PDFF to measure your liver fat and stiffness.
- Calculate your FIB-4 score - it’s free and based on simple blood tests.
- Set a realistic goal: aim for 7-10% weight loss over 6-12 months.
- Work with a dietitian who understands MASLD - focus on whole foods, low fructose, and portion control.
- If you have type 2 diabetes or struggle to lose weight, talk to your doctor about GLP-1 agonists.
- Move every day. Even a 30-minute walk helps.
This isn’t about fixing your liver in a month. It’s about rebuilding your metabolism over time. The science is clear: you can reverse this. And the tools to do it are better than ever.
Can you reverse MASLD without losing weight?
No - weight loss is the only proven way to reverse MASLD. Even GLP-1 drugs work by helping you lose weight and improve metabolism. Without losing fat, especially from the liver and belly, inflammation and scarring won’t improve. Some medications can help reduce liver fat slightly without major weight loss, but they don’t match the results of 10%+ weight reduction.
Are GLP-1 drugs safe for the liver?
Yes - they’re actually beneficial. Early concerns about liver damage were based on rare case reports, not large studies. Multiple trials now show GLP-1 drugs reduce liver fat, inflammation, and even fibrosis. They’re among the safest and most effective treatments for MASLD. The main risks are gastrointestinal side effects, not liver toxicity.
How long do you need to take GLP-1 drugs for MASLD?
There’s no set end date. MASLD is a chronic condition tied to metabolism. Once you stop the drug, weight and liver fat often return. Think of it like blood pressure or diabetes medication - you take it as long as you need to maintain health. The goal is to use it long enough to build lasting habits, then possibly reduce the dose or stop - but only if you’ve permanently changed your lifestyle.
Do I need a liver biopsy to diagnose MASLD?
No. Biopsies are rarely needed anymore. Doctors now use non-invasive tools like FibroScan (which measures liver fat and stiffness) and blood tests like FIB-4. MRI-PDFF is the gold standard for fat quantification. Biopsies are only used if there’s uncertainty about other liver diseases or if advanced scarring is suspected.
Can I take GLP-1 drugs if I don’t have diabetes?
Yes. Semaglutide (Wegovy) and liraglutide (Saxenda) are FDA-approved for weight management in people without diabetes. They’re prescribed for MASLD based on body weight and metabolic health, not blood sugar levels. Many people with MASLD don’t have diabetes - but they still benefit from these drugs because of their effect on fat metabolism and liver inflammation.
Final Thoughts
MASLD isn’t a life sentence. It’s a warning sign - and a chance to reset your health. Losing weight isn’t easy, but it’s the most powerful medicine you can take. GLP-1 drugs aren’t a shortcut, but they’re a powerful tool when paired with real change. The liver is resilient. Give it a chance, and it can heal.





Nupur Vimal
December 15, 2025 AT 23:10they said i needed to lose 10% i lost 18% and now my triglycerides are normal
also stopped my metformin
no more brain fog
just eat less junk and move a bit
Cassie Henriques
December 16, 2025 AT 17:51Michelle M
December 18, 2025 AT 14:22Stop flooding it with sugar.
Stop pretending coffee with syrup counts as breakfast.
Let it breathe.
It's been working overtime for years.
It doesn't need a miracle drug.
It needs you to stop punishing it.
Benjamin Glover
December 19, 2025 AT 04:49Raj Kumar
December 21, 2025 AT 00:15Christina Bischof
December 21, 2025 AT 17:27Mike Nordby
December 22, 2025 AT 20:31John Samuel
December 23, 2025 AT 11:33Sai Nguyen
December 24, 2025 AT 02:15Lisa Davies
December 24, 2025 AT 03:26RONALD Randolph
December 26, 2025 AT 02:07Melissa Taylor
December 26, 2025 AT 07:25John Brown
December 27, 2025 AT 08:53Jocelyn Lachapelle
December 28, 2025 AT 17:40Jake Sinatra
December 30, 2025 AT 01:37