When your nose runs nonstop in spring, or you’re constantly congested all year long, it’s not just a cold - it’s allergic rhinitis. This isn’t just a nuisance. It’s an immune system overreaction to harmless substances like pollen, dust mites, or pet dander. The result? Sneezing, itching, nasal blockage, and watery eyes - symptoms that mess with sleep, focus, and daily life. About 1 in 10 adults in the U.S. have been diagnosed with it, and many more go undiagnosed. The good news? You don’t have to just live with it. There are clear, science-backed ways to manage both seasonal and year-round allergic rhinitis - if you know what to do.
What’s the Difference Between Seasonal and Perennial Allergic Rhinitis?
Not all allergic rhinitis is the same. Seasonal allergic rhinitis, often called hay fever, flares up during specific times of the year. In the UK, that’s usually late March to September. Tree pollen hits in spring, grass pollen peaks in late spring and early summer, and weed pollen lingers into fall. If your symptoms follow the calendar, you’re likely dealing with seasonal triggers.
Perennial allergic rhinitis, on the other hand, sticks around all year. It’s caused by indoor allergens you’re constantly exposed to: dust mites in bedding, pet dander from cats or dogs, cockroach particles in older homes, or mold growing in damp bathrooms and basements. People with perennial rhinitis often feel congested every day, especially in the morning or after being indoors for long periods.
Knowing which type you have matters because it changes your treatment plan. One-size-fits-all doesn’t work here.
First-Line Treatments: What Actually Works
There’s a lot of noise out there - from herbal sprays to nasal rinses - but clinical guidelines agree on what works best. For mild to moderate symptoms, whether seasonal or perennial, oral second-generation antihistamines are a solid start. These include cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra). They work within 1-2 hours, reduce sneezing and itching, and don’t make most people drowsy. A 10 mg dose of cetirizine daily is enough for most adults.
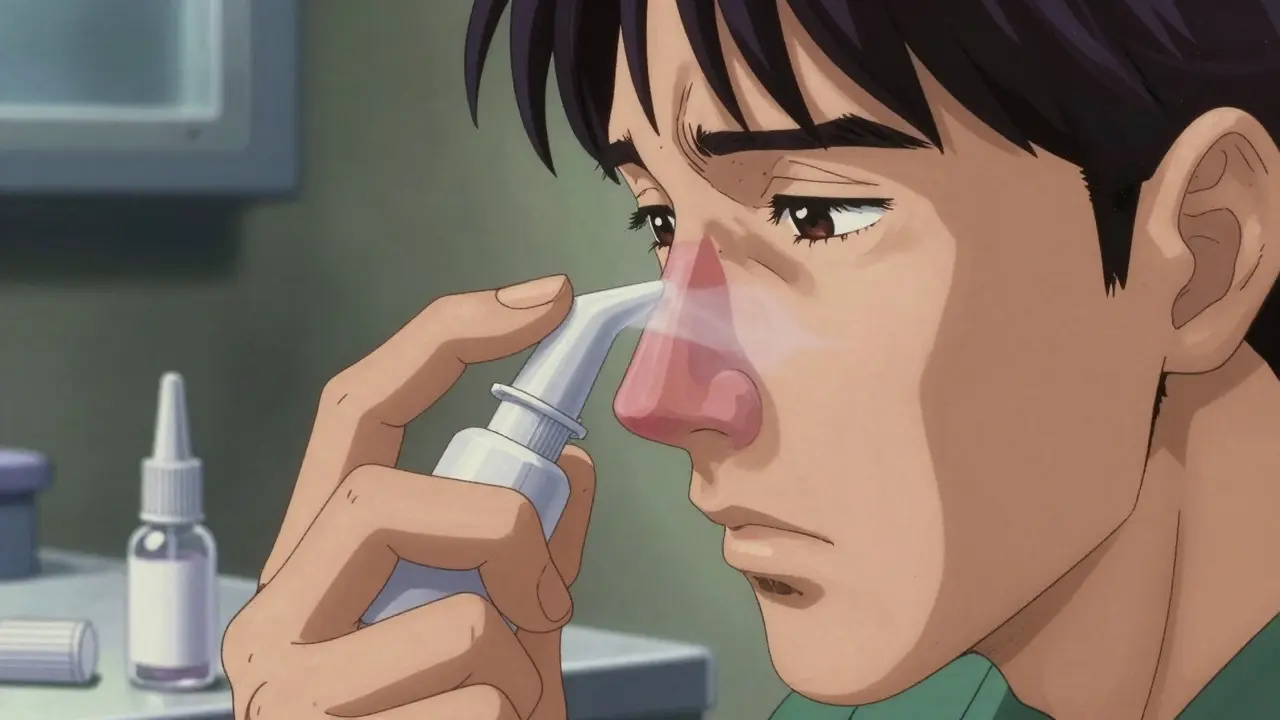
But if you’re struggling with nasal congestion - that stuffed-up, pressure-filled feeling - antihistamines alone won’t cut it. That’s where intranasal corticosteroids come in. These are nasal sprays like fluticasone (Flonase), mometasone (Nasonex), and budesonide (Rhinocort). They’re not instant. You need to use them daily for 1-2 weeks before they fully kick in. But once they do, they reduce inflammation deep in the nasal lining. Studies show they’re 30-50% more effective than oral antihistamines at reducing congestion and overall symptom scores.
Here’s the catch: most people use them wrong. If you point the spray straight up toward the septum (the middle wall of your nose), you’ll get nosebleeds and waste the dose. The right way? Aim slightly outward toward your ear, gently inhale as you spray, and don’t blow your nose for 15 minutes after. Studies show 60-70% of users mess this up - cutting their relief in half.
When Antihistamines and Steroids Aren’t Enough
Some people still struggle even after using the right meds. That’s when you need to think beyond pills and sprays.
Intranasal antihistamines, like azelastine (Astelin), offer fast relief - within 30 minutes. They’re great for sudden sneezing fits or itchy noses. But they’re not as strong as corticosteroids for long-term congestion. They’re often used as a bridge while waiting for steroids to work.
Oral decongestants like pseudoephedrine (Sudafed) can help for a few days if you’re really blocked. But they’re not for daily use. They can raise blood pressure, cause anxiety, and lead to rebound congestion if used longer than 3-7 days.
And then there’s the nasal spray decongestant - oxymetazoline (Afrin). It feels amazing the first time. But use it for more than 3 days straight? You’ll get rhinitis medicamentosa: a cycle of dependence where your nose gets worse the more you use it. It’s a trap many fall into.
Immunotherapy: The Only Treatment That Changes the Game
If you’ve tried everything and still can’t breathe, it’s time to consider immunotherapy - the only treatment that actually reprograms your immune system.
There are two main types: subcutaneous (SCIT), or allergy shots, and sublingual (SLIT), or tablets you place under your tongue. Both work over 3-5 years. SCIT involves weekly shots at first, then monthly maintenance. SLIT is daily tablets you take at home.
SLIT is growing fast. In the U.S., grass pollen tablets like Oralair and Grastek are FDA-approved. They reduce symptoms by 30-40% compared to placebo. They’re easier than shots - no needles, no clinic visits. But they come with a trade-off: 65% of users feel itching or tingling in the mouth, and 32% quit within the first year because of it. You also have to wait 5 minutes after taking the tablet before eating or drinking.
SCIT is slightly more effective - 35-45% symptom reduction - but carries a slightly higher risk of anaphylaxis. That’s why the first shot is always given in a clinic with epinephrine on hand. Both options require long-term commitment. But for people with severe, persistent allergies, they can cut medication use by half and even reduce the risk of developing asthma later on.
Environmental Control: What You Can Do at Home
Medication helps, but if you’re still breathing in allergens, you’re fighting an uphill battle. Here’s what actually works:
- Dust mites: Wash bedding weekly in water hotter than 130°F (54°C). Use allergen-proof covers on your mattress and pillows. This reduces exposure by 83%.
- Mold: Fix leaks. Use a dehumidifier to keep indoor humidity below 50%. Clean bathroom grout with bleach or vinegar monthly.
- Pet dander: Keep pets out of the bedroom. Use a HEPA air purifier. Bathe pets weekly if possible.
- Pollen: Keep windows closed during high-pollen days (over 9.7 grains/m³). Check pollen forecasts daily. Wear wraparound sunglasses outside - they cut eye symptoms by 35%. Shower and change clothes after being outdoors.
Many people skip these steps because they seem too hard. But you don’t need to do everything. Start with one: mattress covers. Then add washing bedding. Small changes add up.
The Role of Nasal Saline Irrigation
Saline rinses - using a neti pot or squeeze bottle with sterile saltwater - aren’t a cure. But they’re a powerful helper. A 2022 survey of 1,200 patients found 62% felt better when they rinsed twice a day, especially when combined with medication. It washes out allergens and mucus, making other treatments work better. It’s cheap, safe, and has no side effects. Just make sure you use distilled or boiled water. Tap water can carry dangerous microbes.
What’s New in 2026?
The field is moving fast. In late 2023, the FDA approved tezepelumab, the first biologic for allergic rhinitis. It blocks a protein called TSLP that kicks off the allergic chain reaction. Early trials showed a 42% drop in symptoms. It’s still expensive and given by injection, but it’s a breakthrough for people who don’t respond to anything else.
Dual-action sprays - like azelastine/fluticasone (Dymista) - are also gaining traction. They combine a fast-acting antihistamine with a steroid in one spray. They work within 30 minutes and reduce symptoms better than either alone. They’re prescription-only but worth asking about if you’re still struggling.
Apps like Pollen Sense are now used in clinics. They give personalized pollen alerts and help users avoid high-exposure days. One study showed 28% better symptom control when people used them with their meds.
Why So Many People Still Struggle
Even with all this knowledge, most people don’t get proper care. Why? Three big reasons:
- They wait too long. The average person waits 3.2 years before seeing an allergist. By then, symptoms are entrenched.
- They stop using steroids too soon. Since they don’t work instantly, 50% of users quit within a year. But the real benefit comes after 2-4 weeks of daily use.
- They don’t get proper instruction. If you’re spraying into the wrong part of your nose, you’re wasting your money.
Don’t be one of them. If you’ve had symptoms for more than a few weeks, see a doctor. Ask about nasal corticosteroids. Ask how to use them right. Ask if immunotherapy could help.
What to Do Next
Start simple:
- Track your symptoms for a week. Do they get worse outdoors? After petting a dog? In the morning?
- Try an OTC antihistamine like cetirizine for 7 days. See if it helps.
- Buy a saline rinse kit. Use it twice a week.
- Get allergen-proof pillow covers. They’re under £15 online.
If that doesn’t help, book an appointment with your GP. Ask for a referral to an allergy specialist. Don’t wait. You don’t have to live with this.
Is allergic rhinitis the same as a cold?
No. A cold is caused by a virus and usually lasts 7-10 days. Allergic rhinitis is triggered by allergens and lasts as long as you’re exposed. Colds often come with a sore throat or fever; allergies cause itching, watery eyes, and clear nasal discharge. If your symptoms keep coming back at the same time each year, it’s likely allergies.
Can children outgrow allergic rhinitis?
Some do, especially if their allergies are mild and triggered by temporary factors like pet dander. But for many, especially those with a family history of asthma or eczema, allergic rhinitis persists into adulthood. Early treatment with immunotherapy can reduce the risk of developing asthma later - one study showed a 67% drop in asthma development after 3 years of treatment in children.
Are nasal steroids safe for long-term use?
Yes. At recommended doses, intranasal corticosteroids have minimal absorption into the bloodstream. Side effects like nosebleeds or dryness are local and rare. They do not cause weight gain, bone loss, or adrenal suppression like oral steroids. The biggest risk is improper use - pointing the spray toward the septum. When used correctly, they’re one of the safest long-term medications available.
Do air purifiers help with allergies?
Yes - but only if they have a true HEPA filter. Cheap ionizers or UV-only purifiers do little. A HEPA filter removes 99.97% of particles as small as 0.3 microns - including pollen, dander, and dust mite fragments. Place it in the bedroom and run it on low overnight. It won’t fix everything, but it helps reduce nighttime symptoms.
Can I use allergy meds while pregnant?
Some are considered safe. Cetirizine and loratadine are Category B - meaning no evidence of harm in studies. Intranasal corticosteroids like budesonide are also low-risk. Avoid decongestants like pseudoephedrine in the first trimester. Always check with your doctor before starting or stopping any medication during pregnancy.