When you’re in pain from arthritis in your knee or hip, a steroid injection can feel like a lifeline. It’s quick, it’s common, and for many, it brings relief within days. But what if that relief comes with hidden costs? Over 12 million of these injections are given in the U.S. every year, mostly for osteoarthritis. Doctors have relied on them since the 1950s, and they’re still widely recommended. But new research is turning the old assumptions upside down.
What Happens When Steroids Leave the Joint
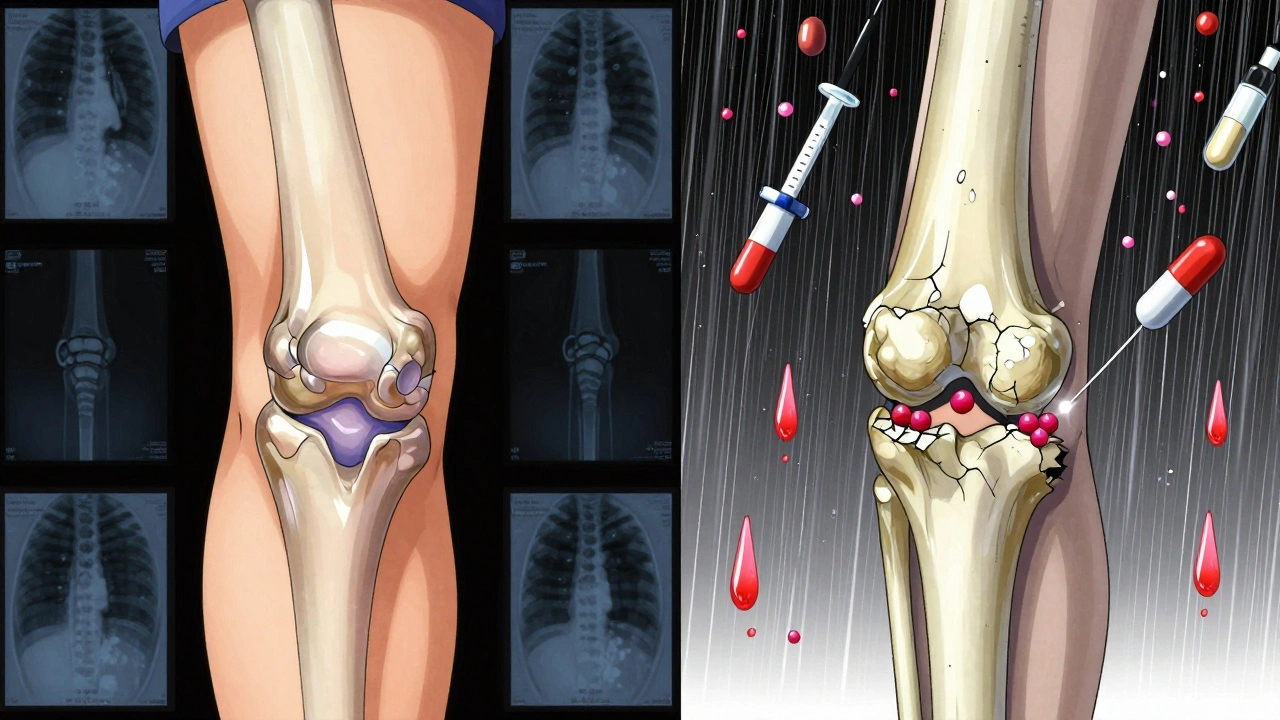
The idea behind intra-articular steroid injections is simple: put the medicine right where it’s needed - inside the joint - and avoid flooding the whole body. That’s the promise. But the reality is messier. Studies show that even when injected directly into a joint, steroids don’t stay there. They leak out. And once they enter the bloodstream, they act like oral steroids: suppressing your adrenal glands, raising blood sugar, increasing blood pressure, and even weakening bones. Take triamcinolone acetonide, one of the most commonly used forms. Research from the American Academy of Physical Medicine and Rehabilitation shows it has particularly high systemic absorption. That means even a single shot can cause cortisol levels to drop for weeks. For someone with diabetes, this can mean dangerous spikes in blood sugar. For someone with osteoporosis, it can mean more bone loss. And for older adults or postmenopausal women - who are already at higher risk - this isn’t just a theoretical concern.The Hidden Damage: Accelerating Joint Breakdown
The biggest shock in recent years? These injections might be speeding up the very problem they’re meant to treat. A 2023 study published in Radiology followed over 1,000 patients with knee and hip osteoarthritis who got steroid shots. The results were alarming: 1% developed rapid joint destruction - including bone death (osteonecrosis), stress fractures under the cartilage, and joint space narrowing of 2 mm or more in just 12 months. That’s not just inflammation. That’s structural collapse. The Osteoarthritis Initiative found patients who got steroid injections were 3.2 times more likely to show worsening on X-rays than those who didn’t. For those who got multiple shots, the risk jumped to 4.67 times higher. Another study showed 44% of patients with hip injections had measurable joint space narrowing after only six months. That’s not a fluke. That’s a pattern. This contradicts older thinking that these injections were harmless if they didn’t relieve pain. Dr. Ali Guermazi, the lead researcher, put it bluntly: “We’ve been telling patients that even if these injections don’t relieve your pain, they’re not going to hurt you. But now we suspect that this is not necessarily the case.”Who’s Most at Risk?
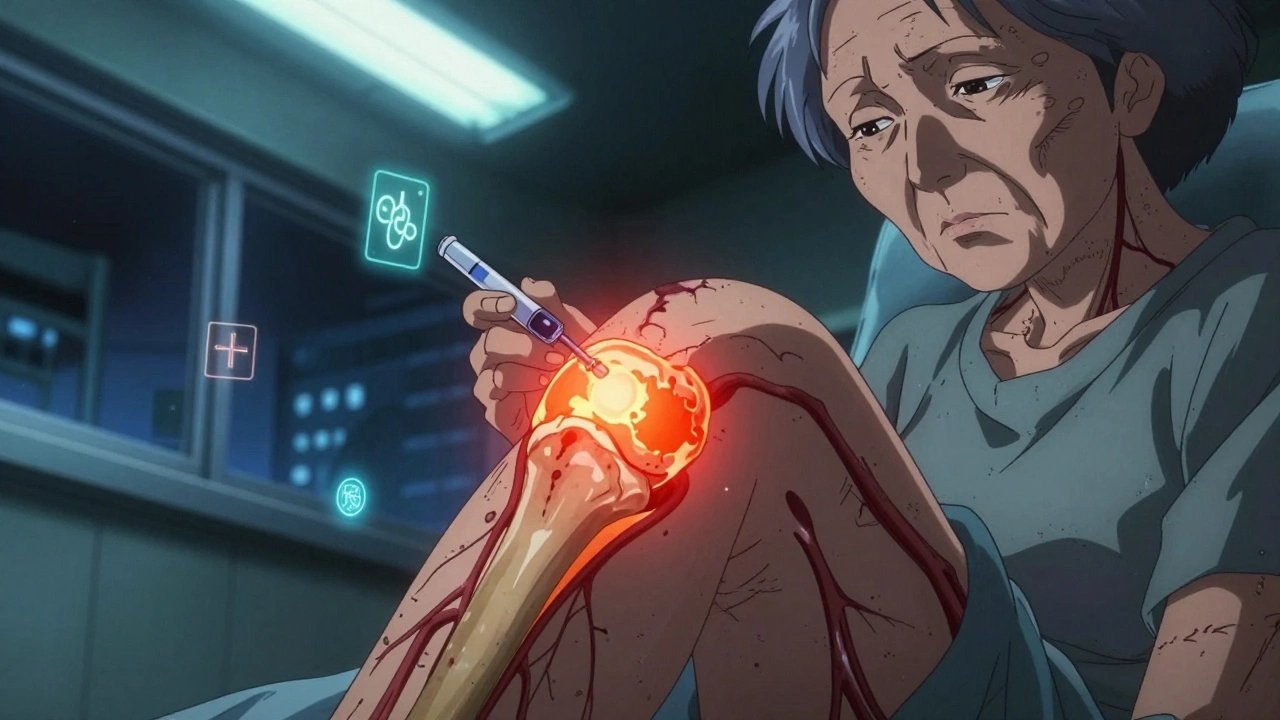
Not everyone reacts the same way. Some people get relief without side effects. Others face serious problems after just one or two shots. Certain groups are far more vulnerable:- People with diabetes - Steroids raise blood sugar. Even a single injection can trigger hyperglycemia for days.
- Postmenopausal women - Estrogen loss already weakens bones. Steroids make it worse.
- Patients with mild osteoarthritis - If your X-ray shows little damage but you’re in a lot of pain, the problem might not be arthritis. Injecting steroids here could mask a more serious issue and accelerate damage.
- Those planning joint surgery - Steroids weaken tissue and delay healing. Getting an injection within 3-6 months of a planned replacement increases complications.
What Are the Real Side Effects?
Let’s be clear: not every side effect is dramatic. Some are mild. Others are life-altering.- Short-term: A flare-up of pain 24-36 hours after the shot (called a steroid flare), swelling, redness, or warmth at the injection site. These usually go away in a couple of days.
- Local damage: Skin thinning, depigmentation (white patches), or fat loss under the skin - especially with injections near the surface, like the elbow or shoulder.
- Systemic effects: High blood pressure, fluid retention, facial flushing, mood swings, trouble sleeping, and elevated blood sugar. These can last for weeks.
- Long-term risks: Adrenal suppression (your body stops making its own cortisol), osteoporosis, increased infection risk, and accelerated joint degeneration.
Why Are They Still Used?
If the risks are real, why are doctors still giving them? Because for many patients, the benefits still outweigh the dangers - at least in the short term. The American Academy of Orthopaedic Surgeons still conditionally recommends steroid injections for knee osteoarthritis. Why? Because the pain relief is real. For someone who can’t walk without help, a few months of mobility might mean the difference between living at home and needing a nursing facility. For older adults with limited options, it’s a tool - not a cure. But here’s the key: it’s supposed to be a temporary solution. Not a long-term crutch. The problem is that many patients and even some providers treat it like a maintenance therapy. That’s where things go wrong.
When Should You Say No?
You don’t need to avoid steroid injections entirely. But you should ask these questions before agreeing:- Is my pain worse than my X-ray shows? If your joint looks okay on imaging but you’re in severe pain, the issue might be something else - like a stress fracture, inflammation from a different source, or even nerve pain. Injecting steroids here could hide the real problem.
- How many have I had in the past year? More than three in one joint? That’s a red flag.
- Do I have diabetes, osteoporosis, or high blood pressure? These conditions make side effects more dangerous.
- Am I planning surgery soon? If you’re thinking about a joint replacement in the next 6 months, skip the shot. It can delay healing and raise infection risk.
- Have I tried other options? Weight loss, physical therapy, braces, and activity modification work for many people. Steroids shouldn’t be the first or only step.
What Are the Alternatives?
There’s growing interest in safer options. Hyaluronic acid injections (viscosupplementation) are sometimes used for knee osteoarthritis. While their benefit is debated, they don’t carry the same systemic risks. Platelet-rich plasma (PRP) and stem cell injections are being studied, but evidence is still limited and they’re expensive. Physical therapy remains the most proven long-term strategy - improving strength, balance, and movement patterns can reduce joint stress and pain without drugs. For people with early osteoarthritis, lifestyle changes - losing even 5-10% of body weight - can cut pain in half. That’s more effective than any injection.The Bottom Line
Intra-articular steroid injections aren’t evil. They’re a tool. But like any tool, they can cause harm if used carelessly. The belief that they’re harmless because they’re “local” is outdated. They enter your bloodstream. They affect your bones. They can speed up joint damage. And for some people, the cost far outweighs the benefit. The goal isn’t to stop all injections. It’s to make smarter choices. Talk to your doctor about your full medical history. Ask about alternatives. Track how many you’ve had. And don’t assume that because it’s a common procedure, it’s risk-free. Your joints may thank you years from now.Can steroid injections cause long-term joint damage?
Yes. Recent studies, including a 2023 study in Radiology, show that repeated intra-articular steroid injections can accelerate joint space narrowing, lead to subchondral fractures, and cause rapid osteoarthritis progression - especially in patients with mild disease or those receiving multiple injections. The risk increases with frequency and dose.
How many steroid injections are safe per year?
Most guidelines recommend no more than 3 to 4 injections per joint per year. However, this isn’t a hard safety limit - it’s based on tradition, not proven safety. For people with diabetes, osteoporosis, or early-stage arthritis, even one or two may carry significant risk. Cumulative exposure matters.
Do steroid injections raise blood sugar?
Yes. Even a single injection can cause blood sugar to rise for several days, especially in people with diabetes or prediabetes. This effect can last up to two weeks. Diabetic patients should monitor their glucose closely for at least a week after the injection and may need to adjust medication temporarily.
Are steroid injections safe before joint replacement surgery?
No. Steroid injections weaken tissues and suppress the immune system, increasing the risk of infection and delaying healing. Most surgeons recommend avoiding steroid injections in the joint for at least 3 to 6 months before planned joint replacement surgery.
What are the signs of systemic side effects after a steroid injection?
Signs include facial flushing, increased thirst or urination, elevated blood pressure, mood changes, trouble sleeping, swelling in the ankles, and unexplained weight gain. If you develop these symptoms within days of the injection, contact your doctor - they may be signs of adrenal suppression or Cushing-like effects.
Do steroid injections help with cartilage repair?
No. Steroid injections reduce inflammation and pain temporarily, but they do not repair cartilage. In fact, evidence suggests they may accelerate cartilage breakdown over time. They are not a disease-modifying treatment - they’re a symptom-management tool.



Christian Landry
December 8, 2025 AT 22:46Katie Harrison
December 9, 2025 AT 03:43Mona Schmidt
December 9, 2025 AT 08:18Guylaine Lapointe
December 10, 2025 AT 08:53Andrea Petrov
December 10, 2025 AT 09:34Suzanne Johnston
December 10, 2025 AT 20:28Graham Abbas
December 12, 2025 AT 01:34Haley P Law
December 13, 2025 AT 04:35ian septian
December 15, 2025 AT 01:05Carina M
December 16, 2025 AT 16:35William Umstattd
December 18, 2025 AT 10:05