Today, more than 90 out of every 100 prescriptions filled in the U.S. are for generic drugs. You probably don’t even think about it when your pharmacist hands you a pill in a plain bottle instead of the colorful box you saw on TV. But this wasn’t always the case. Just 40 years ago, generic drugs were rare, mistrusted, and barely regulated. Their rise to dominance didn’t happen by accident-it took decades of broken promises, deadly mistakes, political battles, and one landmark law that changed everything.
The Roots of Drug Standards: Before Generics Even Existed
Long before anyone talked about generic drugs, the U.S. had no real way to tell if a medicine was safe or even real. In the 1800s, pharmacies sold everything from snake oil to arsenic-laced tonics. In 1820, eleven doctors met in Washington, D.C., and created the first U.S. Pharmacopeia-a list of approved drugs and how they should be made. It was the first step toward standardizing what counted as a real medicine. By 1888, the American Pharmaceutical Association added the National Formulary, which gave pharmacists a reference to spot fake or weak drugs. But these were just guidelines. There were no legal consequences for selling bad medicine. That changed in 1906, when President Theodore Roosevelt signed the Federal Food and Drugs Act. For the first time, companies had to list ingredients on labels. If a drug was dangerous or falsely advertised, the government could step in. Then came the Elixir Sulfanilamide disaster in 1937. A pharmaceutical company dissolved a new antibiotic in diethylene glycol-a toxic antifreeze-to make it easier to swallow. More than 100 people, mostly children, died. Public outrage forced Congress to act. In 1938, the Federal Food, Drug, and Cosmetic Act was passed. Now, drugmakers had to prove their products were safe before selling them. The FDA was given real power. But there was still one big gap: no one had to prove a drug actually worked.The Efficacy Revolution: Kefauver-Harris and the Birth of Modern Regulation
In the early 1960s, the thalidomide crisis in Europe showed what happened when drugs weren’t properly tested. Thalidomide, sold as a sleep aid and morning sickness remedy, caused severe birth defects. Though it never reached the U.S. market in large numbers, the scare pushed lawmakers to act. In 1962, the Kefauver-Harris Drug Amendments changed everything. For the first time, drug companies had to prove their products weren’t just safe-they had to prove they worked. Every new drug had to go through clinical trials. And here’s the kicker: drugs already on the market between 1938 and 1962 had to go back and prove their effectiveness too. Thousands of drugs were pulled or reclassified. This was the moment modern drug regulation was born. But it also created a problem: brand-name companies now had a monopoly on proven, effective drugs. Generics? They were still stuck in the shadows.Why Generics Were Ignored-Until the Money Changed Everything
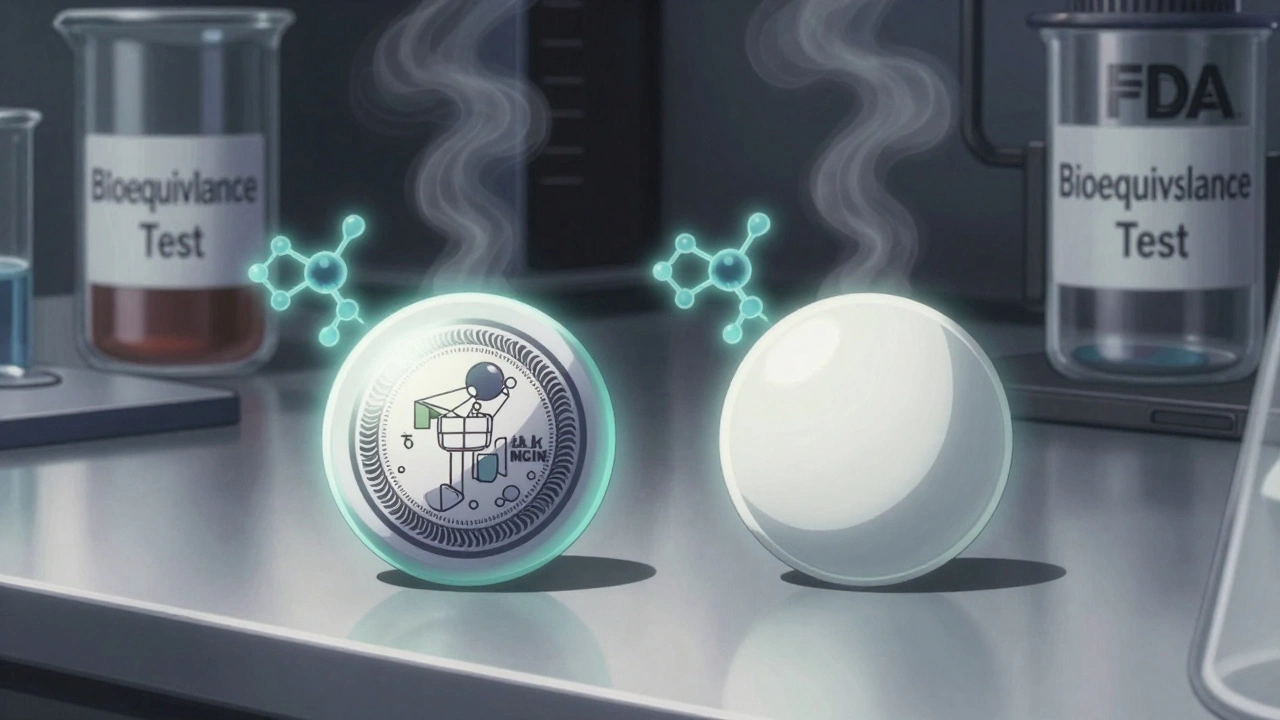
The 1965 Medicaid and Medicare laws changed the game. Suddenly, the federal government was paying for millions of prescriptions. And it didn’t want to overpay. If two drugs had the same active ingredient, why pay five times more for the brand name? But there was no legal way for pharmacies to substitute generics. Doctors didn’t prescribe them. Pharmacists couldn’t switch them without permission. Patients didn’t trust them. In 1984, Congress passed the Drug Price Competition and Patent Term Restoration Act-better known as the Hatch-Waxman Act. This was the turning point. Before Hatch-Waxman, generic companies had to run full clinical trials to prove their drugs worked. That cost millions. It wasn’t worth it. So generics made up only 19% of prescriptions. Hatch-Waxman changed that. It created the Abbreviated New Drug Application (ANDA). Now, a generic company didn’t need to prove safety or effectiveness again. They just had to show their drug was bioequivalent-meaning it released the same amount of medicine into the bloodstream at the same rate as the brand name. That cut development time from years to months and costs from millions to hundreds of thousands. The law also gave brand-name companies a 30-month patent extension if they sued a generic maker. That sounds fair-until you realize it became a loophole. Companies started filing lawsuits not because they believed their patent was being violated, but just to delay competition. Some generic applications sat in limbo for years. The system was supposed to encourage competition. Too often, it was used to block it.
From 19% to 90%: The Explosion of Generic Use
After Hatch-Waxman, things moved fast. By 1990, generics made up 37% of prescriptions. By 2000, it was 50%. Today, it’s 90.5%. The numbers don’t lie. In 2021 alone, generic drugs saved the U.S. healthcare system $373 billion. Over the last decade, that adds up to more than $3.7 trillion. The Congressional Budget Office estimates generics cut drug prices by 80% to 85% compared to brand names. That’s why pharmacies now automatically switch you to generics unless your doctor says no. That’s why your insurance plan charges you $5 for a 30-day supply of metformin instead of $300 for Glucophage. That’s why you can buy 500 pills of lisinopril for less than $10 at Walmart. But here’s the catch: cheaper doesn’t always mean better. Between 2018 and 2022, the FDA recorded 1,234 drug shortages. Sixty-five percent of them involved generic drugs. Why? Because the generic market is built on thin margins. A few companies make a drug. If one factory has a quality issue-or if the price of an active ingredient spikes-supply vanishes. That’s what happened with injectable epinephrine, doxycycline, and even birth control pills. Patients got sick because the cheapest option wasn’t available.Quality, Supply Chains, and the Global Problem
Most of the active ingredients in U.S. generic drugs come from China and India. About 80% of the facilities that make these ingredients are overseas. The FDA inspects them, but they’re spread across thousands of sites. In 2018, an inspection at a plant in India found falsified data. The FDA banned imports. That single event caused shortages of dozens of generic drugs. The FDA’s Generic Drug Program now oversees more than 22,000 generic products and 13,000 manufacturing sites worldwide. Each year, they approve about 900 new generic applications. Since 2012, the Generic Drug User Fee Amendments (GDUFA) have cut review times from 30 months to 10 months and raised approval rates from 45% to 95%. That’s progress. But it’s not enough. In 2019, Congress passed the CREATES Act to stop brand-name companies from blocking access to samples needed for testing. Some companies refused to sell their drugs to generic makers, making it impossible to prove bioequivalence. The FDA has taken 27 enforcement actions under this law since 2019. It’s a start.
What’s Next? Biosimilars and the Next Frontier
The next big wave isn’t going to be pills you can swallow. It’s going to be injections-biosimilars. These are copies of biologic drugs, like Humira or Enbrel, which treat arthritis, cancer, and autoimmune diseases. They cost $100,000 a year. Biosimilars can cut that in half. But they’re harder to make than regular generics. The chemistry is more complex. The FDA has approved fewer than 30 so far. Still, analysts at IQVIA predict biosimilars will be the next major source of savings. By 2027, generics will still make up 90-92% of prescriptions. But biosimilars could take a big bite out of the most expensive drugs on the market.Why This Matters to You
Generic drugs aren’t just a footnote in pharmaceutical history. They’re the reason millions of Americans can afford their prescriptions. They’re why a diabetic can buy insulin for $25 instead of $300. They’re why a heart patient can take their blood pressure pill every day without choosing between meds and groceries. But they’re also fragile. A single factory shutdown, a political dispute over trade, or a price-fixing scheme can leave people without medicine. The system works because of regulation, competition, and oversight. But those things need constant attention. The history of generic drugs in the U.S. is a story of survival-of patients, of public health, and of a system that learned the hard way that medicine shouldn’t be a luxury. The question now isn’t whether we need generics. It’s whether we’re willing to protect them.Are generic drugs really the same as brand-name drugs?
Yes. By law, generic drugs must contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also be bioequivalent, meaning they work the same way in your body. The FDA requires them to meet the same strict quality, purity, and potency standards. The only differences are in inactive ingredients-like fillers or dyes-which don’t affect how the drug works.
Why are generic drugs so much cheaper?
Generic drug makers don’t have to repeat expensive clinical trials to prove safety and effectiveness. Thanks to the Hatch-Waxman Act, they only need to show their product is bioequivalent to the brand-name drug. That cuts development costs dramatically. Plus, once multiple companies start making the same generic, competition drives prices down. Brand-name companies spent years and hundreds of millions developing their drug. Generics skip that step and save consumers 80% to 85% on average.
Can generic drugs cause more side effects?
No. The FDA monitors side effect reports for both brand-name and generic drugs. There’s no evidence that generics cause more side effects. Some patients report differences, but that’s usually due to inactive ingredients-like lactose or dyes-that affect how the pill looks or tastes, not how it works. If you notice a change after switching, talk to your doctor or pharmacist. But it’s rarely because the generic is less safe.
Why do some generic drugs have shortages?
Generic drugs are made on tight profit margins. When only one or two companies make a drug, and one factory has a quality issue, production stops. Many generic manufacturers rely on overseas suppliers for active ingredients. If a plant in China or India shuts down for inspection, or if raw material prices spike, shortages follow. Between 2018 and 2022, 65% of all U.S. drug shortages involved generics. It’s not about safety-it’s about economics.
Is the FDA doing enough to regulate generics?
The FDA has made big improvements. Since 2012, review times for generic applications have dropped from 30 months to 10 months, and approval rates jumped from 45% to 95%. They inspect thousands of overseas facilities each year. But with over 13,000 manufacturing sites worldwide and 900 new applications each year, the workload is enormous. The agency is stretched thin. Enforcement actions under laws like CREATES help, but more funding and international cooperation are needed to keep up.





Kelly McRainey Moore
January 20, 2026 AT 17:13Just got my generic lisinopril for $3 at Walmart yesterday. I used to pay $120 for the brand. No difference in how I feel, just way less stress about my budget. 🙌
Ashok Sakra
January 21, 2026 AT 11:47OMG I HATE GENERICS!! My cousin died because of a bad generic pill!! I know it’s true!! They use rat poison in India!! Why does no one talk about this??
Gerard Jordan
January 21, 2026 AT 15:15Love that we’ve come this far 🌍💊 But let’s not forget - this system only works because real people fought for it. From the Elixir Sulfanilamide tragedy to Hatch-Waxman, it’s not magic, it’s movement. Keep pushing for transparency, y’all! 🙏 #PharmaJustice
Roisin Kelly
January 21, 2026 AT 16:34Yeah right, and I’m supposed to believe that the same pill made in a Chinese factory is magically identical? My anxiety got worse after switching - coincidence? I don’t think so. They’re cutting corners everywhere. And don’t even get me started on the FDA - they’re in the pocket of Big Pharma. Wake up, sheeple.
Yuri Hyuga
January 22, 2026 AT 20:51It’s a remarkable story of how public policy, when guided by compassion and evidence, can transform lives. From the tragedy of 1937 to the triumph of Hatch-Waxman - we didn’t just lower prices, we restored dignity. Millions can now breathe, walk, and live because of this. Let’s not take it for granted. Let’s protect it - not with fear, but with informed advocacy. 💪🌍
Kevin Narvaes
January 23, 2026 AT 08:46bro the generic version of my adderall made me feel like a zombie. i switched back and my brain works again. they’re not the same. they just say they are. lol
Dee Monroe
January 25, 2026 AT 07:48It’s easy to look at the numbers - 90% of prescriptions, $3.7 trillion saved - and feel good. But behind every statistic is someone who waited three weeks for their blood pressure pill because the only factory making it had a quality control issue. Or someone who had to choose between insulin and rent because the generic price jumped 300% overnight. We celebrate efficiency, but we forget fragility. The system works because it’s cheap, not because it’s robust. And when you build something on thin margins and global supply chains controlled by a handful of corporations - you’re not building a safety net, you’re building a house of cards. The real question isn’t whether we need generics - it’s whether we’re brave enough to fund them properly, regulate them honestly, and value human health more than quarterly earnings.