Side Effect Frequency Calculator
Calculate how many people might experience a specific side effect based on the number of people using a drug and the reported frequency. This tool helps you understand why rare side effects only become apparent after a drug is used by millions of people.
When you pick up a new prescription, the prescribing information that comes with it isn’t just a formality. Hidden in Section 6 of that dense document is a critical part called postmarketing experience. This section doesn’t list every possible side effect you might read about online. It doesn’t even include every side effect seen in clinical trials. Instead, it tells you what’s been reported after the drug has been used by hundreds of thousands - sometimes millions - of real people. And understanding what those words mean could make a real difference in your care.
What Exactly Is Postmarketing Experience?
Postmarketing experience is the FDA’s way of capturing side effects that only show up once a drug is out in the wild. Before approval, drugs are tested in clinical trials involving a few hundred to a few thousand people. That’s enough to catch common reactions - nausea, dizziness, headaches - but not rare ones. A side effect that happens in 1 out of 5,000 patients? It’s unlikely to show up in a trial. But once that drug is prescribed to 500,000 people? That’s when you start seeing patterns.
The FDA requires drugmakers to report any serious or unexpected adverse reactions within 15 days of learning about them. These reports go into the FDA’s Adverse Event Reporting System (FAERS), which holds over 35 million entries as of 2023. The information from those reports gets compiled into Section 6 of the drug label - the postmarketing experience section.
Here’s the key: these aren’t confirmed causes. They’re suspected reactions. The label will say things like “reported cases,” “isolated reports,” or “occasionally observed.” That doesn’t mean they’re harmless. It means the link between the drug and the reaction isn’t yet proven beyond doubt - but it’s strong enough to warn doctors.
Why This Section Is Different From Clinical Trial Data
Look at Section 6 and compare it to Section 5 - the clinical trials section. You’ll notice a big difference in tone and detail.
- Section 5 says: “Nausea occurred in 12% of patients.” That’s based on controlled studies with exact numbers.
- Section 6 says: “Nausea has been reported.” That’s based on spontaneous reports from doctors, pharmacists, and patients.
Section 5 tells you what happened under strict conditions. Section 6 tells you what happened in real life - with people taking other medications, with different health conditions, with varying dosages. That’s where the real risks emerge.
Between 2010 and 2020, 62% of serious adverse drug reactions were first detected through postmarketing reports, not clinical trials. That’s according to the Institute for Safe Medication Practices. Think about that: more than half the time, the most dangerous side effects weren’t found until after the drug was already on the market.
What the Words on the Label Really Mean
Here’s where confusion starts. Many clinicians and patients assume that if a side effect is only listed in the postmarketing section, it must be rare or minor. That’s a dangerous mistake.
Take the phrase “isolated reports.” A 2023 review by the American Society of Health-System Pharmacists found that this wording led to underestimation of serious risks. One anticoagulant had 17 fatal bleeding cases labeled as “isolated reports” before the pattern was recognized. “Isolated” doesn’t mean “not serious.” It just means the number of reports is still small - not yet enough to confirm frequency.
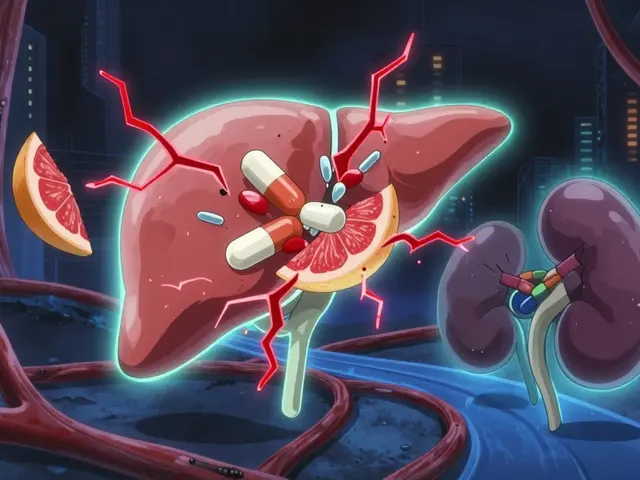
Another common phrase: “reported cases.” This doesn’t mean the drug caused the problem. It means someone reported it after taking the drug. There could be other causes. But if multiple reports come in for the same reaction - especially serious ones like liver failure, heart rhythm changes, or suicidal thoughts - that’s a signal.
And here’s something the FDA explicitly warns about: the absence of a reaction in Section 6 doesn’t mean it doesn’t happen. The label says that outright. Just because it’s not listed doesn’t mean it’s safe.
How Healthcare Providers Use This Info
Doctors don’t just scan Section 6 and move on. When they’re evaluating a new drug, especially for high-risk patients, they look for four things:
- Timing: Did the reaction happen after starting the drug? If it appeared a week in, that’s more likely linked than if it appeared a year later.
- Biological plausibility: Does the reaction make sense based on how the drug works? For example, a drug that lowers blood pressure causing dizziness? Plausible. Causing a rash? Maybe not - unless it’s known to trigger immune reactions.
- Dechallenge-rechallenge: Did the reaction go away when the drug was stopped? Did it come back when restarted? That’s strong evidence.
- Consistency: Are multiple reports showing the same reaction across different patients?
According to a 2022 decision aid from the American College of Clinical Pharmacy, clinicians should spend 3-5 minutes reviewing Section 6 for any new medication - especially if the patient has multiple conditions or is on other drugs.
And here’s the kicker: a 2021 study in the Journal of General Internal Medicine found it takes doctors an average of 18 months to get good at interpreting this data. Even then, specialists are 23% more accurate than generalists. That’s why pharmacists, nurse practitioners, and clinical pharmacologists often play a key role in flagging risks.
Why This Matters for Patients
You might not read the prescribing information. But if you’re on a new medication - especially one that’s been out for less than five years - you should know this: the biggest risks may not be obvious yet.
Some patients report feeling misled when a side effect they experienced isn’t listed in the patient leaflet. But patient leaflets only summarize the most common reactions. The full picture is in the prescribing info - Section 6.
If you’ve had an unusual reaction - say, sudden confusion, unexplained bruising, or chest pain - tell your doctor. Report it to the FDA through MedWatch (Form 3500). Even if your doctor thinks it’s unrelated, your report adds to the data. And if enough people report the same thing, the FDA can update the label.
Between 2022 and 2023, over 42,000 unexpected serious adverse events were reported to the FDA. That’s not noise - that’s early warning.

The Future of Postmarketing Monitoring
This isn’t static. The FDA is moving fast. Starting in January 2025, drugmakers must submit postmarketing data in a machine-readable format called SPL-ESD. That means AI can scan reports in real time, spot patterns, and flag potential new risks faster than ever.
The FDA’s Sentinel Initiative already monitors over 300 million patient records from hospitals and insurers. In 2022 alone, it generated over 1,200 active safety alerts. By 2027, the FDA aims to base 45% of label updates on real-world evidence - up from just 18% in 2022.
Global regulators like the European Medicines Agency have similar systems. That’s why big drug companies now use the same reporting systems for both the U.S. and EU markets. The data is becoming more consistent, more detailed, and more useful.
But technology alone won’t fix the problem. The real challenge is understanding. A 2022 AMA survey found that 63% of physicians are confused by how frequency is presented in Section 6. Forty-one percent assumed reactions listed only in postmarketing sections were less severe. That’s a dangerous assumption.
What You Should Do
Here’s how to use this information wisely:
- Ask your doctor: “Are there any side effects reported after this drug was approved that aren’t in the patient leaflet?”
- Check the full prescribing info: Go to DailyMed (dailymed.nlm.nih.gov) and look up your drug. Go to Section 6. Don’t skip it.
- Report unusual reactions: If you have a side effect that wasn’t listed - especially if it’s serious - report it to the FDA. Your report helps others.
- Don’t assume silence means safety: Just because a reaction isn’t listed doesn’t mean it won’t happen. The label says so.
Postmarketing experience isn’t a warning to avoid a drug. It’s a warning to pay attention. It’s the system working as designed - catching what clinical trials couldn’t. The more we understand it, the safer we all are.
Are side effects listed in postmarketing experience sections less serious than those in clinical trials?
No. Side effects listed only in the postmarketing section are not necessarily less serious. They’re often rare reactions that didn’t show up in clinical trials because those trials involved too few people. A reaction listed as an "isolated report" could still be life-threatening - like liver failure or severe bleeding. The label uses phrases like "reported cases" to indicate uncertainty about whether the drug caused it, not the severity of the reaction.
Why are some side effects listed in both clinical trials and postmarketing sections?
Some side effects appear in both sections because they were seen in trials but became more common or more severe after the drug was widely used. For example, a drug might cause mild dizziness in 5% of trial patients, but after millions are prescribed, doctors report cases of fainting or falls. The postmarketing section adds context - frequency, severity, or new populations affected - that wasn’t clear during trials.
If a side effect isn’t listed in the postmarketing section, does that mean the drug won’t cause it?
No. The FDA explicitly states that the absence of a side effect in the postmarketing section doesn’t mean the drug doesn’t cause it. Many rare reactions take years to appear, or may only occur in people with specific genetic traits or other health conditions. The section only includes reactions that have been reported - not every possible one.
How often are drug labels updated based on postmarketing data?
Between 2007 and 2017, 38% of all drug label updates were due to new safety information from postmarketing experience. In recent years, the FDA has increased its use of real-world data, with over 42,000 unexpected serious adverse events reported in 2022 alone. The agency now aims to base 45% of label updates on real-world evidence by 2027.
Can I report a side effect I experienced?
Yes. Anyone - patients, caregivers, or healthcare providers - can report adverse reactions to the FDA through the MedWatch program using Form 3500. You can file online at fda.gov/medwatch or call 1-800-FDA-1088. Your report helps the FDA identify new safety signals and update drug labels to protect others.


Paul Barnes
January 19, 2026 AT 14:55Postmarketing data isn't a warning-it's a liability shield. Pharma companies know full well that 'isolated reports' means 'we're not legally required to fix this yet.' The FDA's system is broken by design: if it takes 18 months for a doctor to 'get good' at reading Section 6, then the system is failing patients, not helping them.
pragya mishra
January 20, 2026 AT 14:39You people act like this is some noble transparency effort. Newsflash: drug companies report side effects only when forced. The FDA doesn't audit these reports-they just collect them. I've seen patients die because their doctor dismissed 'isolated reports' as 'rare.' That's not safety-it's negligence dressed up as science.
Manoj Kumar Billigunta
January 22, 2026 AT 08:17Let me break this down simply: clinical trials test drugs in healthy, young, mostly white people. Real life? Old people, diabetics, people on 7 meds, people with kidney issues. That’s where the real danger is. Section 6 isn’t fluff-it’s the only thing keeping you alive if you’re not part of the trial group. Don’t ignore it. Talk to your pharmacist. They know this stuff better than your doctor.
Andy Thompson
January 22, 2026 AT 18:56THIS IS A CONTROLLED DEMONSTRATION. The FDA, Big Pharma, and the AMA are all in on it. They want you scared enough to take the pill but not scared enough to question why your liver failed after 3 months. They use 'isolated reports' to bury the truth. And now they're pushing AI to 'scan' it? That’s just a fancy way of saying 'we’re automating the cover-up.' Wake up, people. 🕵️♂️
sagar sanadi
January 23, 2026 AT 11:15So the drug label says 'reported cases' and you think that's a warning? Nah. That's just the industry's way of saying 'we didn't get sued yet.' If it were really dangerous, they'd pull it. But they don't. So it's probably fine. Or maybe they just bought off the regulators again. Either way, your panic is their profit.
kumar kc
January 24, 2026 AT 23:37If you don't read Section 6, you deserve what happens.
Carolyn Rose Meszaros
January 25, 2026 AT 17:24Thank you for writing this. I’ve been telling my mom for years to check DailyMed. She thought the pharmacy leaflet was all there was. Now she reads Section 6 every time she gets a new script. 🙏 It’s wild how few people know this exists.