Medications save lives. But sometimes, they can turn deadly - fast. If you or someone you care about starts having trouble breathing, swelling up, or breaking out in a rash that spreads like wildfire, don’t wait. Don’t call your doctor tomorrow. Don’t check Google. Severe adverse drug reactions are medical emergencies, and every minute counts.
What counts as a severe drug reaction?
Not every rash or stomach upset is dangerous. Mild side effects like drowsiness, dry mouth, or a slight headache are common and usually harmless. But a severe adverse drug reaction is different. It’s not just unpleasant - it’s life-threatening. The U.S. Food and Drug Administration defines a serious reaction as one that causes death, puts someone at risk of dying, requires hospitalization, leads to permanent damage, or causes a disability. These aren’t rare outliers. Anticoagulants, diabetes drugs, and opioids are the top three culprits, according to the U.S. Department of Health and Human Services. They cause bleeding, dangerously low blood sugar, and slowed breathing - all of which can kill if not caught early.Anaphylaxis: The silent killer that strikes in minutes
Imagine taking a pill or getting a shot, and within 10 minutes, your throat starts closing. Your skin breaks out in hives. Your lips swell. You feel dizzy, your chest tightens, and you can’t catch your breath. This is anaphylaxis - a Type I allergic reaction driven by IgE antibodies. It’s the most dangerous kind of drug reaction. It doesn’t wait. It strikes fast. And without treatment, 0.3% to 1% of cases end in death. The key? Epinephrine. Not antihistamines. Not steroids. Not waiting to see if it gets better. Epinephrine, injected into the outer thigh, is the only thing that can reverse this reaction. Dosing is simple: 0.01 mg per kilogram of body weight - up to 0.5 mg for adults. If symptoms don’t improve in five minutes, give another shot. Delaying epinephrine is the most common reason people die from anaphylaxis. The Resuscitation Council UK says it plainly: Don’t wait for a perfect diagnosis. If breathing, airway, or circulation is at risk, give epinephrine now.Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: When your skin starts dying
Then there are the reactions that don’t scream for help - they whisper. A fever. A sore throat. A red, painful rash that spreads. Then the skin begins to blister and peel. This is Stevens-Johnson Syndrome (SJS) or its more deadly cousin, Toxic Epidermal Necrolysis (TEN). These are Type IV reactions - delayed, T-cell driven, and devastating. They often show up 1 to 6 weeks after starting a new drug. Common triggers include antibiotics like sulfonamides, seizure medications like carbamazepine, and painkillers like allopurinol. TEN is terrifying. When more than 30% of your skin detaches, it’s like a severe burn. Infection, fluid loss, and organ failure follow. Mortality hits 30% to 50%. SJS, with less skin loss, still kills 10% of those affected. There’s no quick fix. No epinephrine shot. No home remedy. These patients need intensive care - often in a burn unit. Stopping the drug immediately is the first step. But that’s not enough. You need specialists, IV fluids, wound care, and sometimes immunosuppressants like cyclosporine. If you notice skin peeling after a rash, go to the ER. Don’t wait for it to get worse.
Other dangerous reactions you can’t ignore
Not all severe reactions involve skin or breathing. Some attack your blood. Drug-induced hemolytic anemia or low platelets (thrombocytopenia) can come on days or weeks after taking a drug. You might feel weak, pale, or bruise easily. These are Type II reactions - your immune system attacks your own cells. It’s rare, but deadly if missed. Then there’s DRESS - Drug Reaction with Eosinophilia and Systemic Symptoms. It starts with fever and a rash, but then your liver, kidneys, or lungs get involved. You might feel like you have the flu - but it’s not going away. DRESS can show up 2 to 6 weeks after starting a drug. It’s often misdiagnosed as a virus. But if your liver enzymes spike or your white blood cells go haywire, it’s time to suspect a drug reaction.What to do right now - step by step
If you suspect a severe reaction, act. Here’s what to do:- Stop the drug immediately. Don’t wait for confirmation. If you just took something new and symptoms started, it’s the likely cause.
- Call 999 or go to the nearest emergency room. Don’t drive yourself if you’re dizzy, short of breath, or confused. Get help.
- If you have an epinephrine auto-injector, use it. Inject into the outer thigh. Even if you’re not sure, better safe than dead. You can give a second dose after five minutes if symptoms don’t improve.
- Don’t give antihistamines alone. They help with itching, but they won’t stop anaphylaxis. Epinephrine is the only life-saving treatment.
- Bring the drug bottle. Emergency staff need to know exactly what you took - name, dose, time.
Who needs to carry epinephrine?
If you’ve had a previous severe allergic reaction to a drug - especially anaphylaxis - you should carry an epinephrine auto-injector at all times. Your doctor should give you one and show you how to use it. Practice with the trainer device. Know the expiration date. Keep it with you, not in your car or at home. If you’ve had anaphylaxis to penicillin, sulfa drugs, or contrast dye used in CT scans, you’re at higher risk. Talk to your doctor about getting tested and carrying an injector.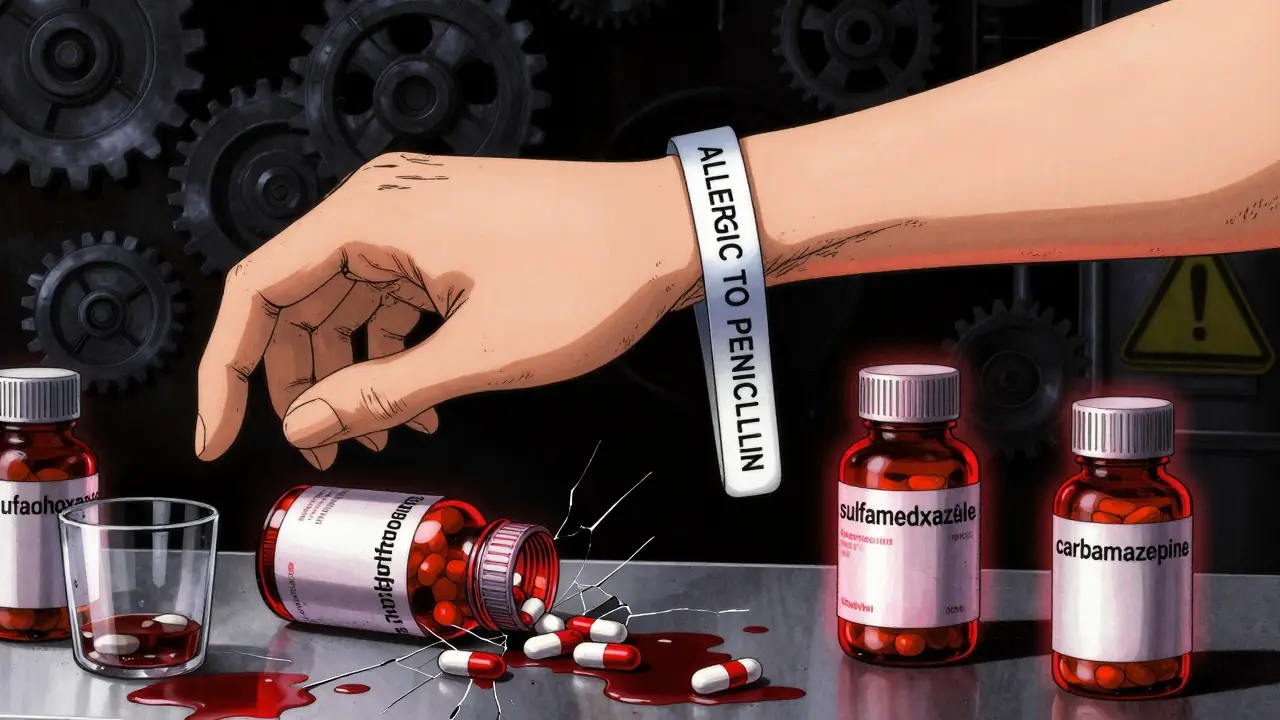
What happens after the emergency?
Surviving a severe reaction doesn’t mean you’re done. You need follow-up. An allergy specialist will help you identify the exact drug that caused it. They may do skin tests or blood tests to confirm the trigger. You’ll get a medical alert bracelet. You’ll learn how to avoid cross-reacting drugs. For example, if you reacted to sulfamethoxazole, you might also react to other sulfa drugs. Your medical records will be flagged. And you’ll get an emergency action plan - written down, clear, and easy to follow.Why most people wait too long
People delay because they think it’s just a rash. Or they don’t want to bother the hospital. Or they believe antihistamines will fix it. Or they think, “It’s never happened before, so it won’t happen now.” That’s the trap. Severe reactions can happen on the first exposure - or the tenth. You can’t predict them. And once you’ve had one, your risk goes up. The American Academy of Family Physicians says: “The first sign of a severe reaction is the time to act - not the third.”How to prevent this from happening again
- Always tell every doctor, dentist, and pharmacist about your drug allergies - even if you think it’s minor. - Keep a written list of all drugs you’ve reacted to, including the reaction type (e.g., “anaphylaxis to penicillin,” “SJS from allopurinol”). - Wear a medical alert bracelet. - Ask for alternatives. If you’re allergic to a common drug, there’s almost always another option. - Don’t take someone else’s medication - even if it’s the same name. Different brands or doses can trigger reactions.Medications are powerful. They can heal - or harm. Knowing the difference between a side effect and a life-threatening reaction can save your life or someone else’s. If you’re ever in doubt - act fast. Epinephrine saves lives. Emergency care saves skin. And never, ever wait to see if it gets better.
Can a drug reaction happen the first time you take a medication?
Yes. While some reactions build up over time, severe ones like anaphylaxis can happen on the very first exposure. Your immune system may have been sensitized earlier through hidden exposure - like trace amounts in food or environmental sources. Never assume a drug is safe just because you’ve taken it before without issue.
Is it safe to use an epinephrine auto-injector if I’m not sure it’s an allergic reaction?
Yes. Epinephrine is extremely safe when used correctly. Even if you’re wrong and it’s not anaphylaxis, the risks of not using it far outweigh the risks of using it. Side effects like a racing heart or shaking are temporary and far less dangerous than untreated anaphylaxis. The guidelines say: when in doubt, use it.
Can I treat a severe drug reaction at home?
No. Severe reactions require emergency medical care. Even if epinephrine helps temporarily, the reaction can come back hours later. Hospital staff monitor for complications like low blood pressure, heart rhythm problems, or lung swelling. Home care is not enough - and it’s dangerously risky.
What drugs are most likely to cause severe reactions?
The top three high-risk drug categories are anticoagulants (like warfarin or rivaroxaban), diabetes medications (especially insulin or sulfonylureas), and opioids (like morphine or oxycodone). For allergic reactions, penicillin, sulfa drugs, NSAIDs (like ibuprofen), and chemotherapy agents are common triggers. Severe skin reactions are often linked to antibiotics, anticonvulsants, and gout medications like allopurinol.
How long after taking a drug can a severe reaction occur?
It depends on the type. Anaphylaxis hits within minutes to two hours. Skin reactions like SJS/TEN can take 1 to 6 weeks to appear. Blood disorders may show up after several days. DRESS syndrome usually appears 2 to 6 weeks after starting the drug. Never assume you’re safe just because symptoms haven’t shown up yet.
Do I need to report a severe drug reaction?
Yes. Reporting helps protect others. In the UK, you can report through the Yellow Card Scheme run by the MHRA. In the U.S., use the FDA’s MedWatch system. Even if you’re not sure the drug caused it, report it. Thousands of reactions are reported each year - and many lead to safety updates, new warnings, or even drug withdrawals.
Can I get tested to find out which drugs I’m allergic to?
For some drugs, yes. Skin tests are available for penicillin and a few others. Blood tests can help with certain types of reactions, like those involving eosinophils. But for many severe reactions - especially SJS/TEN - there’s no reliable test. The best tool is your medical history. Keep a detailed record of what you took and what happened. That’s the most valuable information for your doctor.
If I had a reaction to one drug, will I react to others in the same class?
Sometimes. If you had anaphylaxis to penicillin, you’re likely to react to other penicillin-type antibiotics. But not always. For example, if you reacted to sulfamethoxazole (a sulfa antibiotic), you may also react to other sulfa drugs like furosemide or some diabetes pills. But reactions to NSAIDs like ibuprofen don’t always mean you’ll react to aspirin. Always check with an allergy specialist before assuming cross-reactivity.




Anna Weitz
December 28, 2025 AT 04:27So you take a pill and your skin starts peeling off like a bad sunburn and you're like oh cool guess I'm a human candle now
Nikki Thames
December 29, 2025 AT 07:50It is imperative to underscore that the failure to administer epinephrine within the critical window constitutes a gross negligence of medical protocol. The persistence of antihistamine reliance among laypersons reflects a profound epistemological deficit in public health literacy.
Chris Garcia
December 30, 2025 AT 01:08In my village in Nigeria, we say: when the body rebels against medicine, it is not the medicine that is wrong - it is the soul that is crying out. This post is not just medical advice, it is a sacred warning. Epinephrine is not a drug - it is a lifeline woven by science into the fabric of survival. Carry it. Know it. Use it. Your life is not yours to gamble with.
James Bowers
December 30, 2025 AT 07:32The assertion that epinephrine should be administered without hesitation is clinically sound, yet the omission of contraindications such as uncontrolled hypertension or pheochromocytoma undermines the rigor of this guidance. A responsible medical communication must include nuance.
Will Neitzer
December 30, 2025 AT 12:55Every single word here matters. This isn't just information - it's a blueprint for survival. If you're reading this and you've ever been told 'it's probably just a rash' - please, stop. That's the lie that kills. Epinephrine doesn't fix everything, but it buys you the one thing you can't get back: time. And time is the only currency that matters when your airway is collapsing.
Janice Holmes
December 31, 2025 AT 01:35MY SKIN WAS PEELING OFF IN SHEETS AND I THOUGHT IT WAS A NEW BODY WASH. I WAS IN THE ER FOR THREE WEEKS. THEY SAID IF I'D WAIT ONE MORE DAY I WOULD'VE LOST MY LIVER. I'M STILL SCARED TO TAKE ASPIRIN. DON'T BE THE PERSON WHO WENT TO THE GROCERY STORE INSTEAD OF THE HOSPITAL.
Robyn Hays
January 1, 2026 AT 20:10I love how this breaks down the science without drowning you in jargon. I used to think if I didn’t break out in hives right away, I was fine - turns out my immune system was just plotting. I now carry my epinephrine in my purse, my gym bag, even my kid’s backpack. Better to be the weirdo with the auto-injector than the ghost in the obituary.
Liz Tanner
January 2, 2026 AT 14:29I’m a nurse and I’ve seen too many people wait because they didn’t want to be a burden. You’re not a burden. You’re someone who’s alive because you acted. If you’re unsure - go. Bring the bottle. Say ‘I think this drug is killing me.’ They’ll believe you. I promise.
Kishor Raibole
January 4, 2026 AT 04:26While the Western medical paradigm rightly emphasizes epinephrine and emergency intervention, one must not overlook the holistic dimension of drug-induced pathology. In Ayurveda and Traditional Chinese Medicine, such reactions are viewed as manifestations of deep systemic imbalance - the drug merely the catalyst. To treat only the symptom - the anaphylaxis, the necrolysis - without addressing the underlying doshic or qi disruption is akin to plugging a dam with one’s fingers while the river floods the entire valley. Prevention, therefore, lies not only in avoidance but in purification, balance, and ancestral wisdom.