Taking five or more prescriptions at once isn’t unusual - it’s becoming the norm for older adults. About 41% of people over 75 are managing that many medications, and 15% are taking ten or more. It’s not because they’re overmedicated - it’s because they’re managing multiple chronic conditions like high blood pressure, diabetes, arthritis, and heart disease. The problem isn’t the number of pills, but the risk that they’ll clash. One wrong combination can cause dizziness, kidney damage, internal bleeding, or even a stroke. The good news? You don’t have to live in fear. With the right system, you can take all your meds safely - and even simplify your routine.
Start with a complete, updated medication list
Before you do anything else, write down every single thing you take. Not just prescriptions. Include over-the-counter painkillers, vitamins, herbal supplements, and even antacids. Many dangerous interactions happen because patients forget to mention the ginkgo biloba or the daily aspirin they think doesn’t count. Your list needs four key details for each item: the name (brand and generic), the dosage (like “Lisinopril 10mg”), the time of day (e.g., “take with breakfast”), and the reason (e.g., “for cholesterol”).Don’t rely on memory. Use a notebook, a spreadsheet, or a free app like Medisafe. Update it every time your doctor changes a dose or adds a new pill. Bring this list to every appointment - even if you’ve seen the same doctor before. Studies show that patients who use a written list reduce their risk of dangerous interactions by nearly half.
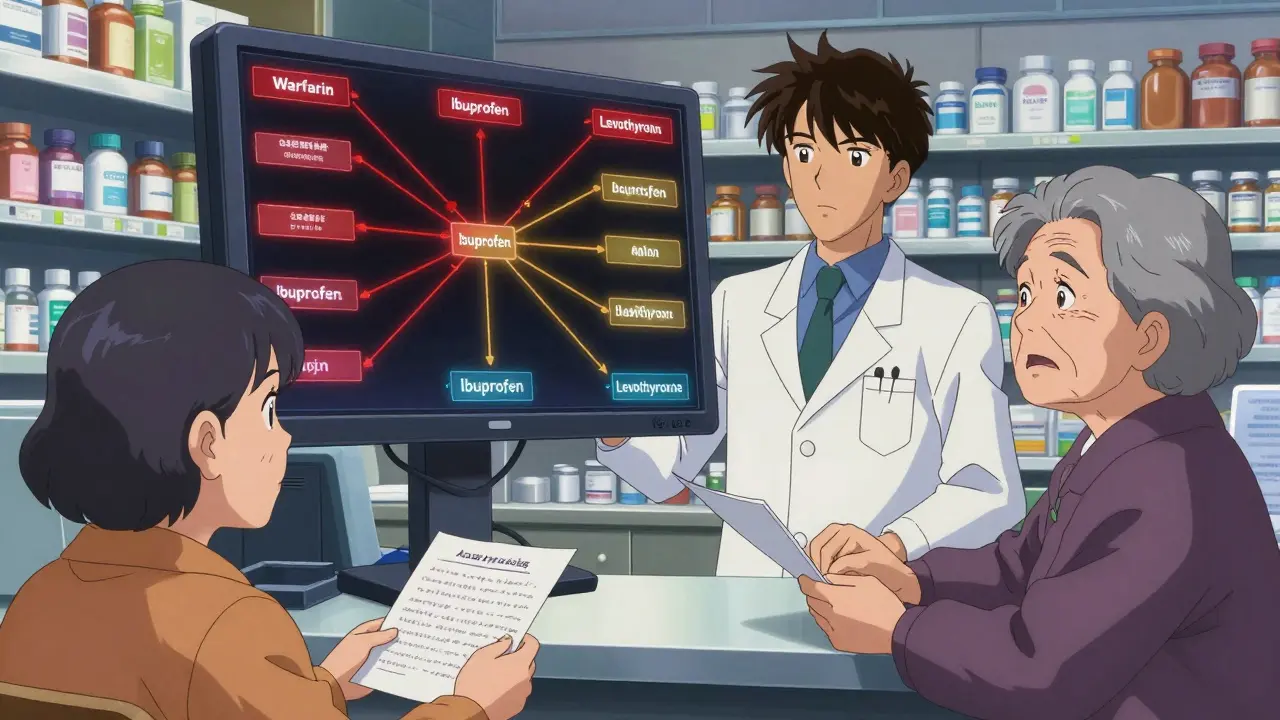
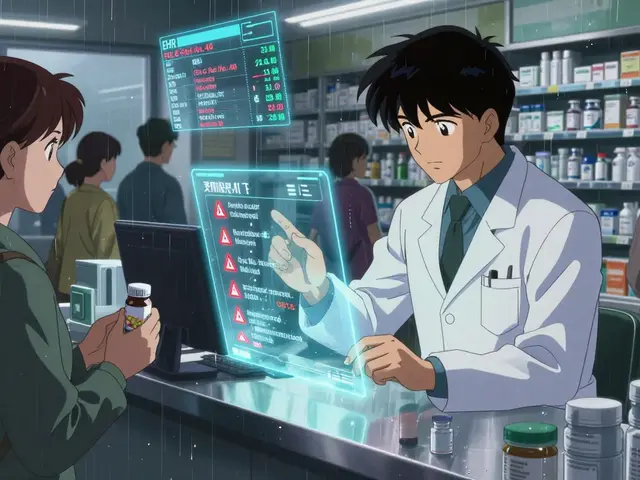
Use one pharmacy for everything
Splitting prescriptions between CVS, Walgreens, and a local pharmacy sounds convenient - until a pharmacist can’t see your full history. A 2023 Health Affairs study found that single-pharmacy users are 47% more likely to catch a dangerous drug interaction than those using multiple pharmacies. Why? Because one pharmacist has your complete record. They can spot that your blood thinner and your new NSAID for arthritis could cause internal bleeding. Or that your cholesterol drug and a common antacid reduce each other’s effectiveness.Pharmacists aren’t just dispensers - they’re medication detectives. Ask your pharmacist to run a full interaction check every time you pick up a new prescription. Most will do it for free. If you’ve been using multiple pharmacies, switch to one now. It’s the single easiest way to cut your risk.
Try medication synchronization
Imagine picking up all your monthly meds on the same day - say, the second Tuesday of every month. That’s medication synchronization. It’s not just about convenience. It’s about safety. When your refills are aligned, you’re less likely to run out of one pill and start taking another out of order. It also means your pharmacist reviews your full regimen every time you pick up.Here’s how it works: You tell your pharmacy you want to sync your prescriptions. They identify which ones are maintenance (daily) vs. as-needed (like painkillers). Then they adjust refill dates so everything lines up. It usually takes 2-3 weeks to set up. Once done, you get one bag with all your meds, ready for the month. Studies show patients in sync programs have 31% fewer missed doses and 22% fewer emergency room visits. Medicare Part D even covers this for people taking eight or more medications for two or more chronic conditions.
Use a pill organizer - the right way
A simple plastic box with compartments for morning, afternoon, evening, and night isn’t just for seniors. It’s for anyone taking more than three pills a day. A 2023 study in the Journal of General Internal Medicine followed 1,245 people over six months. Those using a 7-day AM/PM organizer improved adherence from 62% to 87%. That’s not just a number - it’s fewer hospital stays, fewer side effects, and better control of your conditions.Don’t just buy any organizer. Get one with clear labels and separate compartments for each time of day. Fill it every Sunday evening - make it part of your routine, like watching your favorite show. If you’re forgetful, get one with an alarm. Devices like Hero Health cost around $900, but many insurance plans cover them for high-risk patients. The key? Don’t skip refilling it. If you’re going on vacation, pack your organizer - don’t rely on local pharmacies.
Watch for timing and food interactions
It’s not just what you take - it’s when and how. Some medications need to be taken on an empty stomach. Others must be taken with food. Get it wrong, and the drug won’t work - or worse, it could harm you.For example: Thyroid medication (like levothyroxine) must be taken alone, at least 30-60 minutes before breakfast. If you take it with calcium, iron, or even coffee, your body won’t absorb it. Same with proton pump inhibitors like omeprazole - they need to be taken 30 minutes before your first meal to block stomach acid properly. Calcium supplements should be spaced at least two hours apart from thyroid meds or antibiotics like ciprofloxacin.
Also avoid grapefruit with certain statins and blood pressure drugs. It can cause dangerous spikes in drug levels. Alcohol can make sedatives, painkillers, and antidepressants more powerful - and more dangerous. Always ask your pharmacist: “Is there anything I shouldn’t eat, drink, or take with this pill?”
Ask about deprescribing
Just because a pill was prescribed a year ago doesn’t mean you still need it. Many older adults keep taking medications long after their original purpose is gone - like a muscle relaxant for a healed back injury, or a sleep aid used for a short-term stress episode. The American Geriatrics Society says regularly reviewing and stopping unnecessary meds - called deprescribing - is one of the most effective ways to reduce risk.Ask your doctor: “Is this medication still helping me? Are there side effects I should watch for? Could I take less or stop it?” Don’t be afraid to say no. If a pill causes dizziness, fatigue, or confusion, it might be doing more harm than good. Your pharmacist can help you build a plan to safely taper off, if needed.
Use digital tools - but know the limits
Apps like Medisafe, MyMeds, or CVS’s reminder system send alerts when it’s time to take a pill. They’ve been shown to boost adherence by 28%. But here’s the catch: 62% of adults over 75 don’t use smartphones regularly. If you’re not tech-savvy, a paper list and a pill organizer work better than an app you’ll never open.If you do use an app, make sure it lets you add supplements and OTC meds. Some only track prescriptions. Also, never rely on an app alone. Always cross-check with your written list and your pharmacist. Technology helps - but it doesn’t replace human review.
Know the red flags
Some side effects aren’t normal - they’re warnings. If you start feeling unusually tired, confused, dizzy, nauseous, or have unexplained bruising or dark stools, don’t brush it off. These could be signs of a drug interaction. Dry mouth and constipation are common, but if they’re new or worse, ask your pharmacist. Eighty-two percent of dangerous interactions involve undisclosed supplements. If you’ve started taking turmeric, magnesium, or melatonin, tell your provider. They might not ask.The American Geriatrics Society lists 30 high-risk combinations to avoid in older adults. One common example: combining an NSAID like ibuprofen with a blood thinner like warfarin. It can cause serious stomach bleeding. Another: taking multiple drugs that cause drowsiness - like a sleep aid, an antihistamine, and an antidepressant - which increases fall risk dramatically.
What to do next
You don’t need to fix everything at once. Start today:- Make a complete list of every medication, supplement, and OTC drug you take.
- Go to one pharmacy - and bring your list.
- Ask if they offer medication synchronization.
- Get a 7-day pill organizer and fill it this Sunday.
- Ask your doctor: “Which of these meds can I stop or reduce?”
Every step reduces risk. And the payoff? Fewer hospital visits, better sleep, more energy, and peace of mind. Medication coordination isn’t about being perfect - it’s about being smart. With the right system, you can take control - not just of your pills, but of your health.
What’s the most common mistake people make with multiple prescriptions?
The biggest mistake is using multiple pharmacies. When prescriptions are spread across different stores, no single pharmacist has your full history. That means they can’t catch dangerous interactions between your blood pressure med, your arthritis pill, and your new antibiotic. Using one pharmacy gives you a safety net - pharmacists there can see everything and warn you before a problem happens.
Can I just stop a medication if I think it’s not helping?
No. Stopping some meds suddenly can cause serious problems - like rebound high blood pressure, seizures, or withdrawal symptoms. If you think a pill isn’t working or is causing side effects, talk to your doctor or pharmacist first. They can help you safely taper off or switch to something better. Never quit cold turkey.
Do I really need to tell my pharmacist about vitamins and supplements?
Yes. Supplements aren’t harmless. Garlic, ginkgo, and fish oil can thin your blood and interact with warfarin. St. John’s wort can make antidepressants, birth control, and even heart meds less effective. Over 80% of dangerous interactions involve supplements patients don’t mention. Your pharmacist needs the full picture to keep you safe.
How often should I review my medications?
At least once every six months - or whenever your doctor adds or changes a prescription. Your needs change over time. A pill that helped a year ago might not be needed now. A new condition might mean an old med is now risky. Regular reviews are the best way to avoid unnecessary drugs and catch problems early.
Is medication synchronization covered by insurance?
Many insurance plans, including Medicare Part D, cover medication synchronization for patients taking eight or more medications for two or more chronic conditions. Even if it’s not covered, most community pharmacies offer it for free as part of their care services. Ask your pharmacist - it’s worth checking.
What if I live in a rural area and have to see multiple doctors?
It’s harder, but not impossible. Keep your own master list - updated after every visit. Share it with each provider. Ask each doctor to note which meds they’re prescribing and why. If possible, pick one pharmacy you trust and ask them to contact your doctors to confirm your full list. Many rural pharmacies now offer medication therapy management (MTM) visits - a 20-30 minute session where a pharmacist reviews everything with you. Request one.



John Ross
January 4, 2026 AT 21:46The pharmacokinetic interactions here are non-trivial, especially with CYP450 substrate drugs like statins and calcium channel blockers. Polypharmacy in geriatrics isn't just about pill count-it's about metabolic burden. You're looking at hepatic clearance saturation, renal excretion thresholds, and protein-binding displacement cascades. If you're on warfarin and toss in NSAIDs or even high-dose fish oil, you're flirting with INR spikes that can land you in the ER. The single-pharmacy model isn't a suggestion-it's a pharmacovigilance imperative.
And don't get me started on how Medicare Part D formularies create artificial fragmentation. Pharmacies are incentivized to push generics, but they don't coordinate with prescribers. That's systemic failure dressed up as cost containment.
Clint Moser
January 6, 2026 AT 01:36they said use one pharmacy but did u kno that all the big chains share data with the gov and the big pharma? theyre tracking ur meds to push more pills or to flag u for insurance audits. i got my meds from 3 diff places just so they cant build a full profile. also ginkgo biloba? that stuff is banned in 12 countries for a reason. they say its 'natural' but its a blood thinner that kills ppl and no one talks about it. the system wants u dependent. trust no one. even ur pharmacist.
ps. my aunt died after her 'safe' med sync program. they gave her 3 extra pills she didnt need. they called it 'optimization'. i call it murder by algorithm.
Aaron Mercado
January 6, 2026 AT 07:14And yet-here we are-still letting Big Pharma and the Medicare bureaucracy dictate how we manage our own bodies! This isn’t 'coordination'-it’s institutionalized pharmaceutical control! They want you dependent! They want you on ten pills because it’s more profitable than curing you! You think your 'pill organizer' is helping? It’s a prison for your autonomy! They’ve turned health into a subscription service-and you’re paying monthly with your liver, your kidneys, your dignity!
And don’t even get me started on 'deprescribing'-that’s just a fancy word for 'we’re cutting your meds because your insurance won’t cover another year of them!' I’ve seen it: elderly folks dropped off statins, then dropped dead from a heart attack six weeks later. Who’s to blame? The doctor? The pharmacist? Or the system that treats human beings like data points?
Don’t trust the 'studies.' They’re funded by Pfizer. Don’t trust the 'apps.' They’re spyware with a timer. Don’t trust the 'synchronization.' It’s just another way to make you predictable. You’re not a patient-you’re a product. Wake up.
Vikram Sujay
January 6, 2026 AT 19:30While the practical recommendations offered are sound and evidence-based, I would urge a deeper philosophical reflection on the nature of medicalization in aging. The normalization of polypharmacy as 'the new norm' reflects a societal tendency to pathologize longevity rather than to optimize holistic well-being. The emphasis on systems, tools, and compliance may inadvertently reinforce a biomedical model that overlooks nutrition, movement, social connection, and psychological resilience as foundational to health.
One might ask: if 41% of those over 75 are managing five or more medications, is the problem the number of pills-or the lack of preventive, community-centered care? The pharmacist is indeed a 'medication detective,' but perhaps we need more 'health detectives'-those who ask not only what you are taking, but why you are suffering, and whether healing might lie beyond the pill bottle.
Still, the structural advice-single pharmacy, synchronization, clear lists-is indispensable in our current system. One must navigate the machine, even while questioning its design.
Jay Tejada
January 8, 2026 AT 00:44lol at the 'medication synchronization' thing. sounds like a fancy way of saying 'we’re gonna make you pick up all your pills on Tuesday so we don’t have to work on Friday.'
but honestly? i’ve been using a pill box for 3 years and it’s the only reason i’m still alive. my grandpa used to take his blood pressure med with coffee and wonder why he passed out at the grocery store. now he takes it with water at 7am sharp. no app. no fancy tech. just a plastic box and a cup of tea.
also-yes, tell your pharmacist about the turmeric. they’ve seen it all. they won’t judge you. unlike your cousin who thinks 'natural' means 'safe.'
Shanna Sung
January 8, 2026 AT 02:26EVERYONE IS BEING MANIPULATED. THEY WANT YOU TO THINK YOU’RE IN CONTROL WITH YOUR PILL BOX AND YOUR APPS BUT THE PHARMACIES ARE TRACKING EVERYTHING. THEY KNOW WHEN YOU SKIP A Dose. THEY KNOW WHEN YOU’RE RUNNING LOW. THEY SELL THAT DATA TO INSURANCE COMPANIES SO THEY CAN RAISE YOUR PREMIUMS. AND THE DOCTORS? THEY’RE PAID BY THE NUMBER OF PRESCRIPTIONS THEY WRITE. THAT’S WHY THEY WON’T LET YOU STOP ANYTHING. YOU’RE A CASH COW. YOU’RE A NUMBER. YOU’RE NOT A PERSON.
THEY EVEN USE GINKGO AND MELATONIN TO MAKE YOU DEPENDENT. THEY KNOW YOU’LL TAKE IT BECAUSE IT’S 'NATURAL.' IT’S A TRAP. I SAW A WOMAN IN THE WAITING ROOM TAKE 17 PILLS. SHE WAS 72. SHE DIDN’T NEED HALF OF THEM. NO ONE TOLD HER. NO ONE CARES.
Allen Ye
January 10, 2026 AT 02:18Let’s not reduce this to a checklist of administrative hacks. The real issue here is the fragmentation of care in an aging population under a profit-driven healthcare system. The fact that we need a 'medication synchronization' program at all is a symptom of a system that treats the body as a collection of discrete pathologies rather than a unified organism. We’ve outsourced agency to pharmacists, apps, and pill organizers because we’ve abandoned longitudinal, relationship-based medicine.
When your primary care physician knows you by name, when they’ve watched you lose your spouse, when they remember you stopped taking that beta-blocker because it made you too tired to garden-that’s when deprescribing becomes ethical, not bureaucratic. The single-pharmacy model? Good. The pill organizer? Necessary. But none of it replaces the human who remembers your story.
And yes, grapefruit and statins? Classic. But why are we still prescribing statins to 80-year-olds with no history of cardiac events? That’s not medicine-that’s algorithmic inertia. We’re treating risk factors like diseases. We need to stop prescribing for data points and start prescribing for people.
mark etang
January 10, 2026 AT 07:42Excellent, comprehensive guide. This is precisely the kind of evidence-based, actionable advice that empowers patients to take ownership of their health outcomes. The integration of clinical best practices with real-world operational strategies-such as medication synchronization and single-pharmacy utilization-demonstrates a sophisticated understanding of systems-level barriers to adherence.
I commend the author for emphasizing deprescribing as a core competency in geriatric care. Too often, the default is continuation rather than critical reassessment. This paradigm shift-from accumulation to intentional stewardship-is not merely prudent; it is a moral imperative in an era of escalating polypharmacy-related morbidity.
Healthcare professionals and patients alike must treat medication regimens as dynamic, evolving protocols-not static scripts. Thank you for elevating the discourse.
josh plum
January 10, 2026 AT 08:55You people are so naive. You think using one pharmacy makes you safe? Nah. That’s just the first step they want you to take so they can lock you into their ecosystem. You think your pharmacist gives a damn about you? They’re paid by the hour to fill scripts, not to save lives. And 'medication synchronization'? That’s just a fancy way of saying 'we’re gonna make sure you never miss a dose so we can keep billing Medicare.'
And don’t even get me started on supplements. You take 'natural' stuff? You’re basically handing Big Pharma a free pass to poison you. Ginkgo? Turmeric? Those are just gateway drugs to the real stuff. They want you dependent. They want you scared. They want you to think you need 10 pills to live.
Here’s the truth: most of these meds aren’t for you-they’re for the shareholders. Stop being a good little patient. Ask for less. Demand less. You’re worth more than a pill bottle.
Brendan F. Cochran
January 10, 2026 AT 15:22Y’all are overthinking this. Just go to one pharmacy, use a pillbox, and stop taking all that junk. I’m 78 and I take 6 pills. I don’t need an app. I don’t need a spreadsheet. I just do it. My wife died because she was on 14 meds and never told anyone about her ginkgo. Don’t be her. Simple. Done.
Also, grapefruit? Dumb. Just don’t eat it. Why is this even a thing? It’s not rocket science. Stop making it complicated. America’s problem isn’t polypharmacy-it’s overcomplication.
jigisha Patel
January 12, 2026 AT 12:44The empirical data presented is methodologically sound, yet the underlying assumptions remain uninterrogated. The recommendation to use a single pharmacy presupposes equitable access to pharmaceutical infrastructure, which is demonstrably false in rural and low-income urban settings. Furthermore, the emphasis on patient compliance ignores the cognitive load imposed by polypharmacy on individuals with mild cognitive impairment-a population that constitutes nearly 40% of those over 75.
The 'pill organizer' solution assumes intact executive function, which is neither universal nor guaranteed. The absence of caregiver-inclusive strategies renders this framework exclusionary. Moreover, deprescribing protocols are inconsistently implemented across specialties; without standardized clinical decision support tools, recommendations remain aspirational rather than actionable.
In sum: the advice is technically correct but socially naive.
Jason Stafford
January 14, 2026 AT 01:29THEY’RE LYING TO YOU. EVERY SINGLE THING IN THIS POST IS A COVER. THE PHARMACISTS? THEY’RE WORKING FOR THE GOVERNMENT. THE PILL BOXES? THEY HAVE TRACKERS INSIDE. THE 'FREE INTERACTION CHECKS'? THEY’RE JUST GATHERING DATA TO PUT YOU ON A WATCHLIST. YOU THINK THEY WANT YOU HEALTHY? THEY WANT YOU CONTROLLED. THEY WANT YOU DEPENDENT. THEY WANT YOU TO BELIEVE YOU NEED ALL THESE PILLS SO YOU NEVER QUESTION WHY YOU’RE SO TIRED, SO CONFUSED, SO SICK.
WHY DO YOU THINK THEY PUSH 'MEDI SAFE' AND 'HERO HEALTH'? BECAUSE THEY CAN SEE WHEN YOU SKIP A DOSE. BECAUSE THEY CAN TELL YOUR INSURANCE YOU’RE NONCOMPLIANT. BECAUSE THEY CAN RAISE YOUR PREMIUMS. BECAUSE THEY CAN DENY YOU CARE.
STOP TRUSTING THE SYSTEM. START TRUSTING YOUR BODY. IF YOU FEEL BAD, STOP THE PILLS. NOT THE DOCTOR. NOT THE PHARMACIST. YOU. YOUR BODY KNOWS. THEY DON’T.
John Ross
January 14, 2026 AT 12:00Re: Jason Stafford’s rant about trackers in pill organizers-completely fabricated. Hero Health devices use Bluetooth for refill alerts and medication adherence logging, not surveillance. The data is encrypted, HIPAA-compliant, and owned by the patient. No third party gets access without explicit consent.
But your paranoia isn’t baseless. The real surveillance is in the formulary restrictions and prior authorizations that force patients into certain drugs. That’s the system’s control-not the pill box.
And yes, deprescribing is hard. But it’s not because of conspiracy. It’s because medical training doesn’t teach it. We’re trained to add, not subtract. That’s the failure. Not the pill organizer.