OTC Drug Interaction Checker
Check Your Medication Safety
This tool helps identify potential interactions between your medications and common health conditions. Remember: OTC drugs can interact dangerously with prescription medications and certain health conditions.
When a medicine moves from prescription-only to over-the-counter (OTC), it seems like a simple win: easier access, lower cost, no doctor’s visit. But behind that convenience is a real shift in risk. You’re no longer under a doctor’s watch. You’re now responsible for knowing when to use it, how much to take, and what else you’re taking that might clash with it. And that’s where things can go wrong.
Why Do Medications Switch from Prescription to OTC?
The goal isn’t to make drugs cheaper or more profitable - though those happen too. It’s about giving people safe, proven treatments for common problems without needing a doctor every time. Think of ibuprofen. Back in the 1980s, you needed a prescription. Now, you grab it off the shelf next to pain relievers and antacids. Why? Because decades of data showed it was safe for most people when used as directed for headaches, muscle aches, or fever. The FDA approved the switch after reviewing thousands of patient reports, side effect studies, and usage patterns. The same happened with loratadine (Claritin), omeprazole (Prilosec OTC), and even some nasal decongestants. The pattern? The condition has to be easy to self-diagnose - like a runny nose, heartburn, or mild pain. The drug needs a wide safety margin. And the label? It has to be clear enough that someone with no medical training can follow it. But here’s the catch: just because it’s OTC doesn’t mean it’s harmless. It means it’s less risky - not risk-free.The Hidden Dangers of Self-Medication
People often treat OTC drugs like candy. They grab a pill because they feel off. They take two because one didn’t work fast enough. They mix it with another OTC product they’re already using. And they never think to check if it’s safe with their other meds. Take acetaminophen. It’s in more than 600 OTC products - cold medicines, sleep aids, allergy pills, and pain relievers. If you take two different products that both contain it, you can easily hit the toxic limit. Liver damage doesn’t always come with warning signs until it’s too late. One Reddit user, PharmTech2020, shared how they saw patients double-dose OTC pain meds because they didn’t realize both products had the same active ingredient. NSAIDs like ibuprofen and naproxen are another silent threat. Long-term use can lead to stomach ulcers, kidney damage, or even heart attacks - especially in people with high blood pressure, diabetes, or kidney disease. And if you’re already on blood thinners? That risk spikes. The FDA warns that mixing aspirin with anticoagulants can cause dangerous bleeding. Yet, most people never think to ask a pharmacist. Even something as simple as a decongestant like pseudoephedrine can be dangerous. If you’re taking an antidepressant like an MAOI or a tricyclic, it can send your blood pressure through the roof. One nurse on Reddit reported multiple cases of elderly patients on blood pressure meds who developed severe hypertension after starting OTC decongestants - no doctor consulted, no warning read.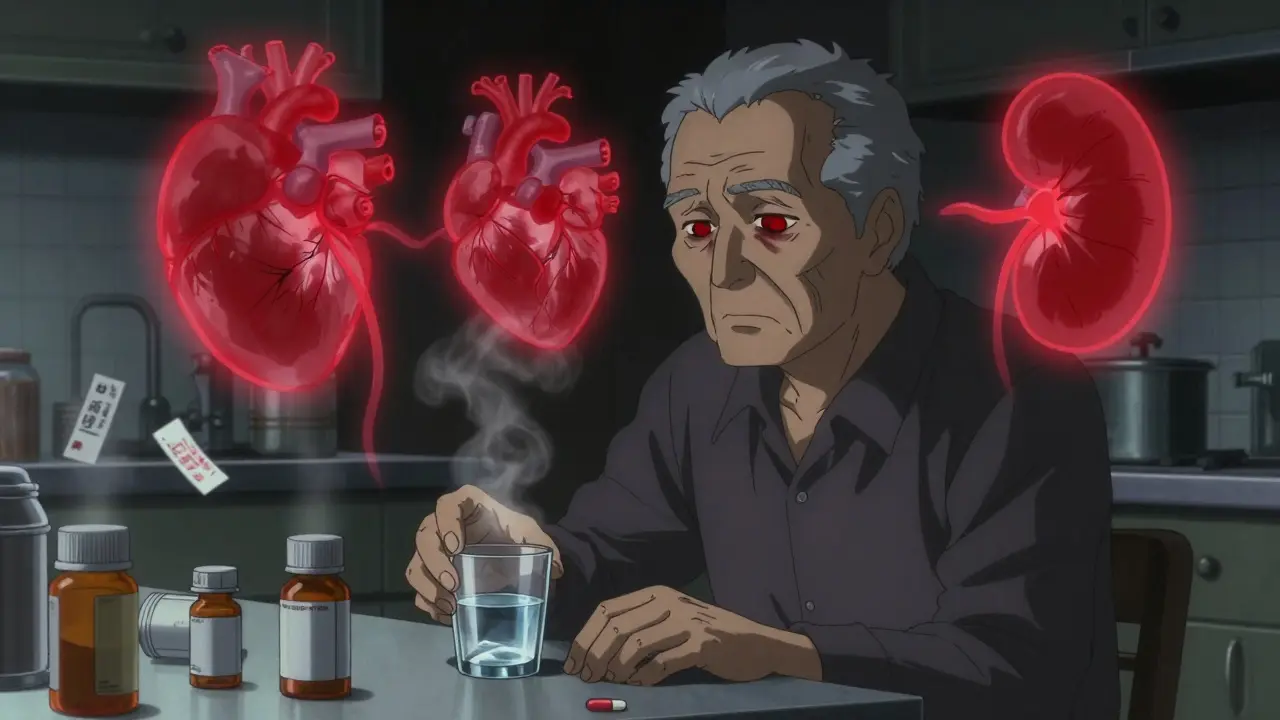
Who’s Most at Risk?
Not everyone handles OTC drugs the same way. Certain groups are far more vulnerable. Older adults are at the top of the list. Their bodies process drugs slower. They often take five, six, or more medications daily. The American Geriatrics Society lists 30 OTC drugs that are risky for people over 65. Diphenhydramine (found in Benadryl and many sleep aids) can cause confusion, dizziness, and falls. NSAIDs increase stomach bleeding risk by 2 to 4 times in this group. Children are another concern. Parents might think, “It’s just a kids’ cold medicine,” but dosing by weight matters. Giving the wrong amount can lead to overdose. And some OTC cough and cold medicines aren’t even recommended for kids under 6. People with chronic conditions - asthma, diabetes, heart disease, liver or kidney problems - need extra caution. An OTC drug that’s fine for a healthy person might worsen their condition. A diabetic taking an OTC decongestant might see their blood sugar spike. Someone with kidney disease might not realize NSAIDs can cause acute kidney failure. And then there’s the problem of misdiagnosis. You think it’s a cold, but it’s sinusitis. You think it’s heartburn, but it’s a heart issue. OTC meds mask symptoms - they don’t fix the root cause. Delaying real medical care because you’re treating the symptom can be deadly.How to Use OTC Drugs Safely
You don’t need to avoid OTC drugs. You just need to treat them like real medicine. Step 1: Read the Drug Facts label. Not the front. Not the brand name. The back. The Drug Facts label is required by the FDA and tells you exactly what’s in it, what it’s for, what to avoid, and how to use it. Look for the “Warnings” section. Does it say “Do not use if you have high blood pressure”? Then don’t use it if you do. Step 2: Check for duplicate active ingredients. Write down every medication you’re taking - prescription, OTC, supplements. Compare the active ingredients. If two things say “acetaminophen” or “ibuprofen,” you’re doubling up. That’s not better. That’s dangerous. Step 3: Talk to your pharmacist. They’re not just the person handing you the box. Pharmacists are trained to spot interactions. If you’re on three or more medications, ask them to review everything you’re taking - even the OTC stuff. A 2022 survey found only 32% of people consistently read the full label. But 68% do talk to a pharmacist before buying. Use that resource. Step 4: Know your limits. If a symptom lasts more than a few days - or gets worse - stop taking the OTC drug and see a doctor. Don’t keep increasing the dose. Don’t “try one more time.” Your body is sending a signal.




Amy Le
January 7, 2026 AT 03:23Joann Absi
January 7, 2026 AT 06:09Mukesh Pareek
January 8, 2026 AT 20:59Jeane Hendrix
January 10, 2026 AT 03:46Leonard Shit
January 11, 2026 AT 19:17Gabrielle Panchev
January 13, 2026 AT 03:05Venkataramanan Viswanathan
January 13, 2026 AT 07:47Kiran Plaha
January 14, 2026 AT 19:56