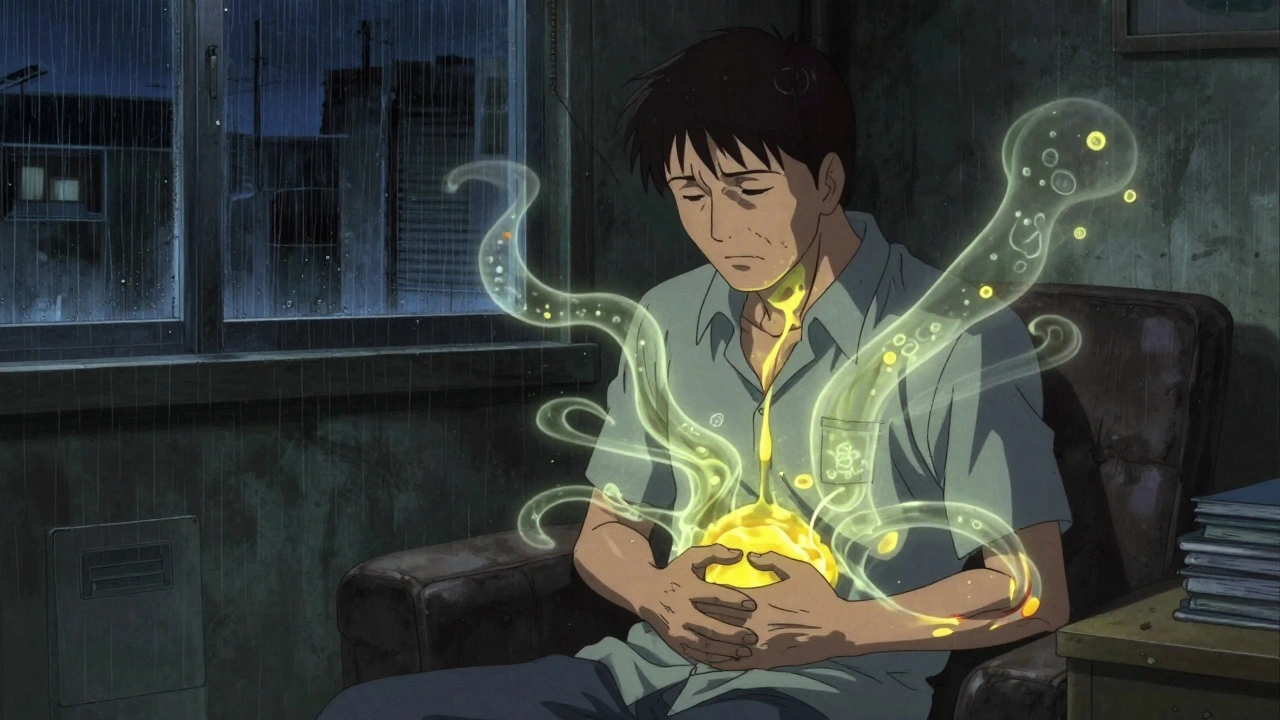
Primary Sclerosing Cholangitis (PSC) isn’t something most people hear about until it hits close to home. It’s a rare, slow-burning disease that attacks the bile ducts-tiny tubes that carry digestive fluid from the liver to the intestines. Over time, these ducts become scarred, narrowed, and blocked. Bile can’t flow properly. The liver gets damaged. And without a cure, the disease keeps moving forward, often silently, until it’s too late.
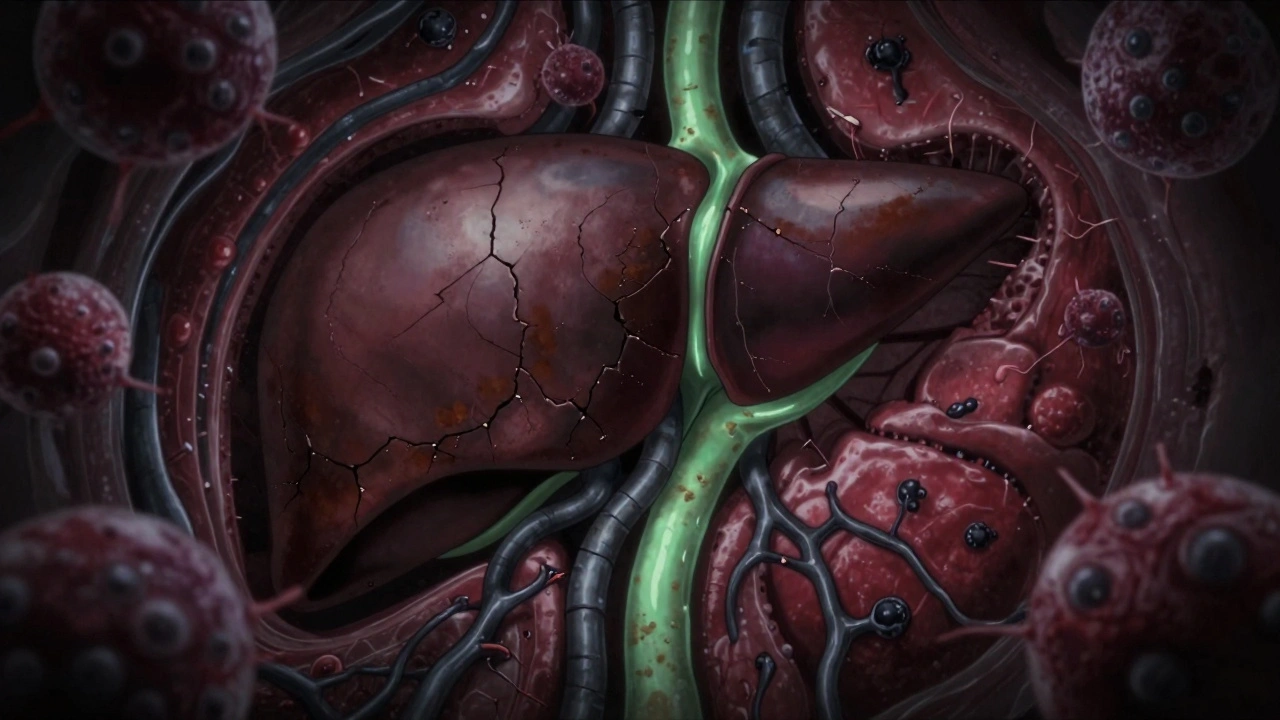
What Happens Inside the Body With PSC?
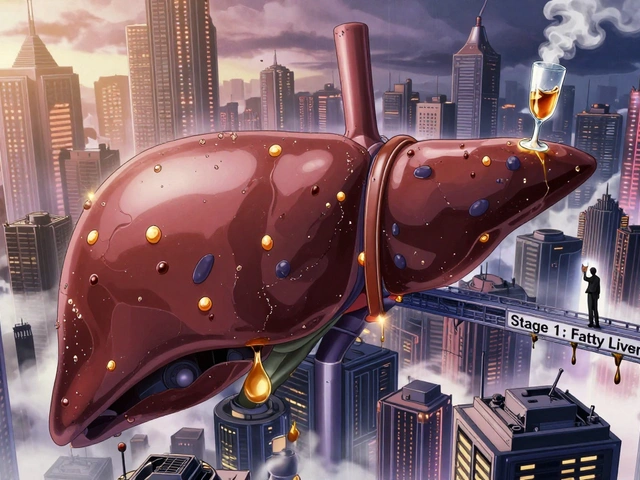
Your liver makes bile to help digest fats. That bile travels through ducts, both inside and outside the liver, to reach the small intestine. In PSC, the immune system turns against those ducts. It doesn’t know why, but inflammation starts. Scar tissue builds up. The ducts thicken, stiffen, and shrink. Some become so narrow they’re barely visible on imaging-less than 1.5mm wide, compared to normal ducts that are 3 to 8mm. When bile backs up, it poisons liver cells. Over years, that leads to cirrhosis-permanent scarring of the liver.
This isn’t a quick process. For most people, it takes 12 to 15 years from the first symptoms to reach cirrhosis. And even then, many don’t feel anything until the damage is advanced. That’s why PSC is called a silent disease. Fatigue, itching, and mild abdominal discomfort are the early warning signs. But they’re easy to ignore. People chalk them up to stress, aging, or a bad diet. By the time jaundice (yellow skin) or fever shows up, the disease is often already in a dangerous phase.
Who Gets PSC-and Why?
PSC doesn’t pick its victims randomly. It’s mostly men. About two out of every three diagnosed are male. The average age at diagnosis is 40. Most cases happen between 30 and 50. And it’s far more common in people of Northern European descent. In Sweden, it affects 6.3 out of every 100,000 people. Globally, it’s rarer-about 1 in 100,000.
Genetics play a big role. Scientists have found 22 gene locations linked to PSC. The strongest link is a version of the HLA-B*08:01 gene. People with this variant are over twice as likely to develop PSC. But genes alone don’t cause it. Something else has to trigger it. And that something? The gut.
Over 70% of people with PSC also have inflammatory bowel disease, especially ulcerative colitis. The connection isn’t coincidence. The gut and liver are tightly linked. When the gut lining gets damaged, bacteria and their waste products leak into the bloodstream and head straight to the liver. In people with the right genetic background, the immune system mistakes bile duct cells for invaders and starts attacking them. This is called the gut-liver axis-and it’s the leading theory behind how PSC starts.
How Is It Diagnosed?
There’s no single blood test for PSC. Doctors look for clues. Elevated liver enzymes, especially ALP (alkaline phosphatase), are the first red flag. But that can happen in many liver conditions. The real diagnosis comes from imaging. MRCP (magnetic resonance cholangiopancreatography) is the gold standard. It’s a non-invasive scan that shows the bile ducts in high detail, revealing the telltale beading and narrowing caused by scarring.
ERCP (endoscopic retrograde cholangiopancreatography) is another option, but it’s riskier. It involves inserting a scope into the gut and injecting dye into the ducts. It’s used mostly when a blockage needs to be opened right away. Blood tests for p-ANCA (a type of antibody) are positive in about half of PSC patients-but that’s not enough to confirm the diagnosis. Unlike Primary Biliary Cholangitis (PBC), which has a clear antibody marker (AMA), PSC doesn’t have a reliable blood test. That’s why diagnosis often takes years.
Many patients wait 2 to 5 years before getting a correct diagnosis. One Reddit user described it as ‘being told it’s anxiety, then IBS, then maybe gallstones-until someone finally looked at my bile ducts.’
What Are the Real Symptoms?
Symptoms vary wildly. Some people feel fine for years. Others struggle daily.
- Fatigue: Over 90% of patients report this. It’s not just being tired. It’s bone-deep exhaustion that doesn’t go away with sleep.
- Pruritus (itching): Affects nearly 80%. It’s not just skin-deep. Patients describe it as ‘itching from inside my bones,’ especially at night. It can be worse than pain.
- Abdominal discomfort: Usually in the upper right side, dull or achy. Often mistaken for indigestion.
- Jaundice: Yellow skin and eyes. A sign the liver is struggling to process bile.
- Cholangitis: Fever, chills, and severe pain. This is a bacterial infection in the bile ducts-a medical emergency.
And then there’s the emotional toll. A 2023 survey found 62% of patients felt their symptoms weren’t taken seriously. Doctors often have little to offer beyond symptom management. That leaves patients feeling abandoned.
Is There a Cure?
No. Not yet. Liver transplant is the only treatment that can truly stop PSC’s progression. Around 80% of people who get a transplant survive at least five years. But it’s not a perfect fix. PSC can come back in the new liver, though it’s rare. And transplant means a lifetime of immunosuppressants, which bring their own risks.
For years, doctors gave patients high doses of ursodeoxycholic acid (UDCA) to try to improve bile flow. But multiple large studies now show it doesn’t improve survival. In fact, doses above 28 mg/kg/day may actually increase the risk of serious complications. The European Association for the Study of the Liver and the American Association for the Study of Liver Diseases now both say: don’t use UDCA routinely.
So what’s left? Symptom control.
- For itching: Rifampicin (150-300 mg daily) works for about half of patients. Naltrexone (50 mg daily) helps with opioid-related itching. Colesevelam, a bile acid binder, reduces itching by trapping bile in the gut.
- For vitamin deficiencies: PSC blocks fat absorption, so vitamins A, D, E, and K often drop dangerously low. Regular blood tests and supplements are essential.
- For IBD: If you have ulcerative colitis, you need a colonoscopy every 1 to 2 years. PSC raises your lifetime risk of colorectal cancer to 10-15%.
What’s on the Horizon?
There’s real hope now. For the first time, drugs are being tested that might actually slow or stop PSC-not just treat symptoms.
Obeticholic acid, a drug that targets the bile acid receptor FXR, showed a 32% drop in liver enzymes in a major 2023 trial. But the FDA is holding off on approval because of side effects like severe itching. Cilofexor, another FXR activator, reduced liver enzyme levels by 41% in early trials and got orphan drug status in Europe in early 2023.
Other drugs targeting PPAR receptors (which regulate inflammation and metabolism) are also in phase 2 trials. Researchers believe that within five years, we’ll have at least two disease-modifying therapies. That could reduce the need for transplants by 40% in the next decade.
But there’s a dark side: cholangiocarcinoma. That’s bile duct cancer. People with PSC have a 1.5% annual risk of developing it. Once it happens, survival drops to just 10-30% at five years. That’s why regular MRCP scans and tumor marker checks (like CA 19-9) are part of every PSC patient’s routine.
How to Live With PSC
Living with PSC means becoming your own advocate. It’s not just about taking pills. It’s about:
- Getting care at a specialized PSC center. Patients treated at these centers report 85% better symptom control than those seeing general hepatologists.
- Monitoring liver enzymes every 3 months. That’s how you catch changes early.
- Getting annual MRCP scans to track duct changes.
- Working with a dietitian. Fat malabsorption is real. You may need high-calorie, low-fat meals with vitamin supplements.
- Connecting with others. Online communities like PSC Partners Seeking a Cure have over 3,000 members. Hearing someone else say, ‘I feel the same way,’ can be life-changing.
And don’t underestimate the power of a good support system. PSC doesn’t just affect your liver-it affects your sleep, your work, your relationships. Many patients stop working because of fatigue. Others can’t travel because of frequent bathroom needs or fear of infection. You’re not alone in this struggle.
Why Research Funding Is So Low
PSC affects about 25,000 people in the U.S. That’s fewer than ALS or Huntington’s disease. And yet, in 2022, the NIH spent $8.2 million on PSC research. For NAFLD-a much more common liver disease-it spent $142 million. That’s a 17-fold difference.
Because it’s rare, pharmaceutical companies haven’t rushed to invest. But that’s changing. The global PSC drug market is expected to grow from $187 million in 2022 to $432 million by 2029. More trials mean more hope. And more awareness means more funding.
Right now, the best thing you can do-whether you have PSC or know someone who does-is to keep asking questions. Push for specialist care. Demand regular monitoring. Support research. Because for PSC, progress isn’t guaranteed. It’s fought for.
Is primary sclerosing cholangitis the same as primary biliary cholangitis?
No. While both affect bile ducts and cause liver damage, they’re different diseases. Primary Biliary Cholangitis (PBC) mainly attacks small bile ducts inside the liver and is strongly linked to anti-mitochondrial antibodies (present in 95% of cases). PSC affects both large and small ducts, inside and outside the liver, and rarely shows those antibodies. Instead, about half of PSC patients test positive for p-ANCA. PBC is more common in women, while PSC affects men more often. Treatments and progression patterns also differ.
Can PSC be reversed or cured with diet or supplements?
No. There’s no diet, herb, or supplement proven to reverse PSC or stop its progression. While a healthy diet helps manage symptoms and prevent vitamin deficiencies, it doesn’t cure the disease. High-dose vitamin D or milk thistle may sound appealing, but studies show no benefit. In fact, some supplements can harm the liver. Always talk to your doctor before trying anything new.
Why does PSC cause so much itching?
Bile acids build up in the blood when ducts are blocked. These acids stimulate nerve endings in the skin, triggering intense itching. But it’s not just skin-deep-many patients describe it as an internal burning or crawling sensation. The exact mechanism isn’t fully understood, but it’s linked to bile acids activating specific receptors in the nervous system. That’s why drugs like rifampicin and naltrexone, which affect nerve signaling, can help.
How often should someone with PSC get a liver scan?
Annual MRCP scans are recommended to monitor bile duct changes and check for early signs of cancer. Liver enzyme blood tests should be done every 3 months. If symptoms worsen or new ones appear-like fever, sudden jaundice, or weight loss-scans may be needed sooner. Some centers also use ultrasound or elastography to check for liver stiffness, which signals fibrosis.
What’s the risk of liver cancer with PSC?
People with PSC have a 1.5% chance each year of developing cholangiocarcinoma, a deadly cancer of the bile ducts. That adds up to a 10-15% lifetime risk. It’s hard to detect early because symptoms overlap with PSC itself. Doctors use MRCP scans and blood tests for CA 19-9 to monitor risk, but even then, cancer is often found too late. That’s why regular screening and specialist care are critical.
Can you live a normal life with PSC?
Yes-but it requires adaptation. Many people with PSC work, travel, raise families, and live full lives. But they manage fatigue, plan around bathroom needs, take supplements, and stick to regular checkups. The key is early diagnosis, specialist care, and staying informed. With new drugs in trials and better support systems, life expectancy and quality are improving. It’s not easy, but it’s possible.
What Comes Next?
PSC is a disease of frustration. It’s slow. It’s unpredictable. It’s often misunderstood. But it’s not hopeless. Research is moving faster than ever. Patients are speaking up. Clinics are getting better. And for the first time, we’re seeing drugs that might actually change the course of the disease.
If you or someone you know has PSC, don’t wait for the next big breakthrough. Start now: find a specialist, get your scans, join a community, and ask questions. Knowledge is power. And in a disease with no cure, that’s the most powerful tool you have.



Bruno Janssen
December 13, 2025 AT 00:21I’ve been living with this for 8 years. Some days I just stare at the ceiling wondering why my body turned on itself. No one gets it unless they’ve felt that bone-deep itch at 3 a.m. with no relief.
Doctors act like it’s just fatigue. Like I’m lazy. But it’s not. It’s the bile crawling under my skin.
Scott Butler
December 13, 2025 AT 19:20Another rare disease getting taxpayer money while real problems like obesity and diabetes get ignored. Why are we funding this when 1 in 3 Americans are prediabetic? This is just a rich person’s luxury illness.
Emma Sbarge
December 14, 2025 AT 23:16My brother was diagnosed last year. We didn’t know what to do until we found PSC Partners. The specialist he sees now has changed everything. He’s sleeping again. The itching’s under control. It’s not a cure but it’s a life.
Don’t let anyone tell you this isn’t worth fighting for. It is.
Deborah Andrich
December 15, 2025 AT 20:29I’ve read every study on this. The gut-liver axis is the key. We’ve been looking at the liver like it’s the problem when it’s the victim. The real issue is the leaky gut letting bacteria trigger the immune system.
Probiotics won’t fix it. But targeting the microbiome? That’s where the next decade of breakthroughs will happen.
If you’re reading this and you have PSC - you’re not broken. Your body’s just sending a signal we haven’t learned to listen to yet.
Tommy Watson
December 16, 2025 AT 00:25so like... urso is bad now? lol i thought that was the magic pill. my doc still prescribes it like its 2010. and why is everyone so obsessed with transplants? like i dont wanna be on immunosuppressants for life. its crazy.
also why does everyone say 'its silent' when i feel it ALL THE TIME??
Donna Hammond
December 16, 2025 AT 06:13For anyone reading this who’s just been diagnosed: you’re not alone. The fatigue isn’t in your head. The itching isn’t psychosomatic. The frustration? Real.
Get tested for vitamin levels. Start a symptom journal. Find a center that treats PSC regularly - not just any liver doctor. The difference is night and day.
And if your doctor dismisses you? Find another one. Your life depends on it.
sharon soila
December 17, 2025 AT 06:30Every human being deserves dignity in illness. PSC is not a footnote. It is a battle fought in silence by thousands who are told they are imagining it. We must demand more. Not because it is common. But because it is human.
Research funding is not a number. It is a promise. And we are breaking it.
nina nakamura
December 18, 2025 AT 00:33Ursodeoxycholic acid is still being prescribed? That’s medical malpractice. People are dying because doctors are clinging to outdated protocols. This isn’t science - it’s inertia.
And don’t get me started on the 'support groups'. They’re just echo chambers for people who don’t want to face reality. Transplant or die. There’s no middle ground.
Hamza Laassili
December 18, 2025 AT 07:17Wait, so if you have IBD, you’re more likely to get PSC? That’s wild. My cousin had ulcerative colitis and now she’s on the transplant list. I didn’t even know they were connected.
Also, why is this disease so underfunded? It’s not like it’s rare - it’s just not talked about. We need a viral campaign. Like Ice Bucket Challenge but for bile ducts.
Someone make a TikTok. Please.