Warfarin-NSAID Risk Calculator
Calculate Your Bleeding Risk
Based on clinical evidence showing how different NSAIDs interact with warfarin. Select your situation to see your risk level and safety recommendations.
When you're on warfarin, even a simple pain reliever like ibuprofen or naproxen can turn dangerous. This isn't a hypothetical warning - it's backed by decades of clinical data showing that combining warfarin with NSAIDs can spike your risk of serious, even deadly, bleeding. If you're taking warfarin for atrial fibrillation, a mechanical heart valve, or deep vein thrombosis, understanding this interaction isn't optional. It's life-saving.
How Warfarin Works - And Why It's Already a Tightrope Walk
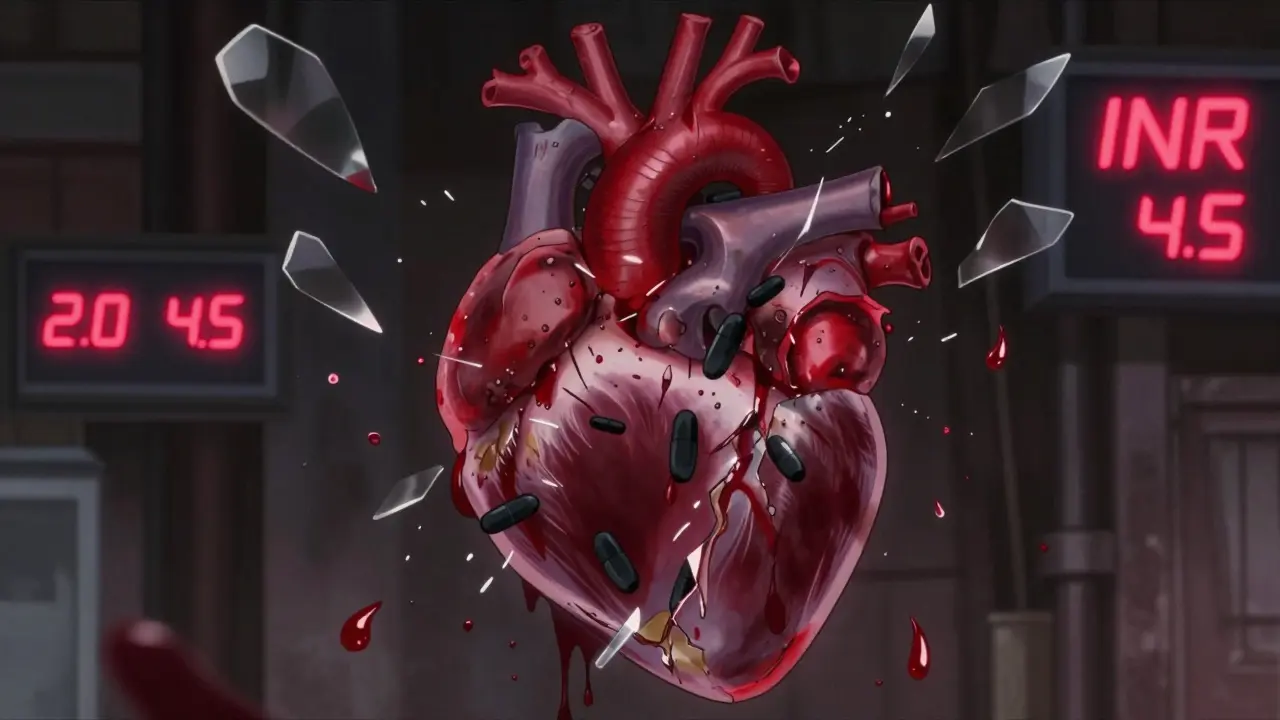
Warfarin doesn't thin your blood like water. It messes with your body's ability to make clotting factors. Specifically, it blocks vitamin K from activating factors II, VII, IX, and X. These are the proteins your body needs to form clots and stop bleeding after an injury. Without enough active clotting factors, your blood takes longer to clot - measured by your INR (International Normalized Ratio). A normal INR is around 1.0. For most people on warfarin, the target range is between 2.0 and 3.0. Go above 4.0? Your risk of spontaneous bleeding jumps sharply.
Keeping INR stable is hard enough on its own. Diet changes, antibiotics, even a new vitamin supplement can throw it off. That’s why most patients get their INR checked every few weeks. Now add an NSAID into the mix, and the stability you’ve worked so hard to achieve? It can vanish in days.
NSAIDs Don’t Just Relieve Pain - They Disrupt Clotting
NSAIDs - like ibuprofen, naproxen, diclofenac, and even low-dose aspirin - work by blocking enzymes called COX-1 and COX-2. COX-2 inhibition reduces inflammation and pain. But COX-1? That’s the one that helps platelets stick together. When NSAIDs block COX-1, they reduce thromboxane A2, a key signal that tells platelets to clump at injury sites. Without it, your blood can’t form a solid plug, even if all your clotting factors are working fine.
This effect is reversible - meaning platelet function returns once you stop the NSAID. But while you’re taking it, your body is fighting a two-front war: warfarin is slowing down clotting factor production, and the NSAID is stopping platelets from doing their job. Together, they create a perfect storm.
The Numbers Don’t Lie - Bleeding Risk Skyrockets
Studies have quantified just how dangerous this combo is. A 2019 analysis from the European Society of Cardiology found that people taking both warfarin and an NSAID had more than double the risk of any major bleeding compared to those on warfarin alone. That’s a 2.09-fold increase.
But not all NSAIDs are created equal. The risk varies:
- Naproxen: 4.1 times higher bleeding risk
- Diclofenac: 3.3 times higher
- Ibuprofen: 1.79 times higher
Even more alarming: the location of bleeding changes. Brain bleeds (intracranial hemorrhage) rose 3.22 times higher. Gut bleeding jumped 2.24 times. And anemia from chronic blood loss? Nearly tripled.
One 2024 meta-analysis confirmed that combining warfarin with NSAIDs doubles the risk of gastrointestinal bleeding - the most common and often most deadly site. This isn’t just a stomach upset. It’s internal bleeding that can lead to shock, transfusions, or death.
Why Some People Are at Even Higher Risk
Not everyone on warfarin who takes an NSAID will bleed. But certain factors make it far more likely:
- High warfarin dose (over 40 mg per week): Your body is already barely holding onto clotting balance. Add an NSAID? The system tips.
- Low baseline INR: If your INR is on the lower end of normal (say, 2.1), you have less room to absorb the extra anticoagulant effect before crossing into danger.
- Other medications: Antibiotics, antifungals, or even some herbal supplements (like garlic or ginkgo) can interact with warfarin too. Add an NSAID? The risk stacks.
- Meloxicam: One study found this NSAID, often prescribed for arthritis, independently increased INR spikes - even more than expected.
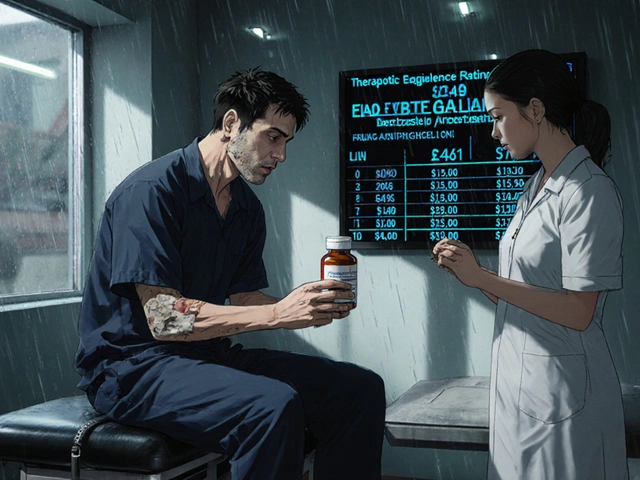
If you’re on high-dose warfarin, taking multiple meds, or have a history of ulcers or GI bleeding - you’re in the highest-risk group. And yet, a 2022 study found nearly 30% of warfarin users got an NSAID prescription within a year. That’s not just a mistake. It’s a systemic failure.
What About Newer Blood Thinners? Are They Safer?
Many patients switch from warfarin to DOACs like apixaban, rivaroxaban, or dabigatran because they don’t need regular INR checks. But here’s the catch: NSAIDs still raise bleeding risk with these drugs too.
A 2018 study found that while dabigatran didn’t interact with NSAIDs *more* than warfarin did, the absolute risk of major bleeding - especially in the gut - still went up significantly in NSAID users. And here’s something surprising: among those taking NSAIDs with DOACs, 60% of major bleeds happened outside the GI tract - meaning brain, lung, or urinary bleeding became more common.
So switching to a DOAC doesn’t make NSAID use safe. It just changes where the bleeding might happen.

What Should You Do Instead?
There are safer ways to manage pain if you’re on warfarin:
- Acetaminophen (Tylenol): Up to 3,000 mg per day is generally safe for most people on warfarin. It doesn’t affect platelets or clotting factors. This is the first-line recommendation from major guidelines.
- Topical NSAIDs: Gels or patches like diclofenac gel applied to the skin (e.g., for knee pain) deliver minimal drug into the bloodstream. This cuts systemic risk significantly.
- Physical therapy: For chronic joint or back pain, movement and strengthening exercises reduce reliance on pills.
- Cold/heat therapy: Simple, non-drug options that help with inflammation and stiffness.
If you absolutely must take an oral NSAID - say, after surgery or for severe arthritis - do it with extreme caution:
- Use the lowest effective dose for the shortest time possible.
- Avoid naproxen and diclofenac. If you must choose, ibuprofen is the least risky - but still risky.
- Take it with food. Never on an empty stomach.
- Ask your doctor about a proton pump inhibitor (PPI) like pantoprazole 40 mg daily to protect your stomach lining.
- Get your INR checked within 3-5 days of starting the NSAID - and again weekly while you’re on it.
What Signs Should You Watch For?
If you’re on warfarin and take an NSAID - even once - you need to know the red flags:
- Bright red blood in stool or black, tarry stools
- Unexplained bruising, especially large or spreading bruises
- Bleeding gums when brushing teeth
- Nosebleeds that won’t stop
- Headaches, dizziness, confusion (possible brain bleed)
- Dark urine or blood in urine
- Unusual fatigue or shortness of breath (signs of anemia from blood loss)
If you notice any of these, stop the NSAID and call your doctor immediately. Don’t wait. Bleeding from this interaction can escalate fast.
The Bottom Line
Warfarin and NSAIDs don’t just interact - they amplify each other’s dangers. The science is clear: combining them increases bleeding risk by up to four times. It’s not a matter of "maybe" or "sometimes." It’s a guaranteed, measurable, and preventable danger.
Most people on warfarin don’t need NSAIDs. Acetaminophen, physical therapy, or topical treatments work just as well for most types of pain - without the risk. If your doctor suggests an NSAID, ask: "Is there a safer alternative?" If they say no, push for a PPI and a follow-up INR test within days.
This isn’t about avoiding pain relief. It’s about choosing relief that doesn’t put your life at risk. When you’re on warfarin, every pill matters. Make sure the one you’re taking isn’t the one that could kill you.




Nikki Brown
December 26, 2025 AT 21:16Wow. Just... wow. I can't believe people still take ibuprofen like it's candy while on warfarin. This isn't rocket science. If you're dumb enough to mix these, you deserve what happens. I've seen three people bleed out from this exact mistake. No excuses. Stop being lazy and use Tylenol. That's it. End of story. 🙄
Peter sullen
December 28, 2025 AT 11:19It is imperative to underscore, with the utmost scientific rigor, that the pharmacodynamic interplay between vitamin K antagonists and non-selective cyclooxygenase inhibitors engenders a synergistic pro-hemorrhagic cascade, wherein both the coagulation cascade and primary hemostasis are concurrently impaired. This is not merely a "risk," but a quantifiable, statistically significant, and clinically actionable interaction that mandates immediate intervention and patient education. Failure to recognize this constitutes a breach of standard-of-care protocols.
Amy Lesleighter (Wales)
December 28, 2025 AT 13:57my grandma was on warfarin for 12 years and never took ibuprofen. she used heat packs and stretching. she said pain was just your body saying slow down. not a reason to pop pills. tylenol’s fine if you need it. but honestly? most of the time, rest works better. no drama. no bleeding. just peace.
Becky Baker
December 28, 2025 AT 16:24Why do we even let these drugs exist if they’re this dangerous? America’s so obsessed with quick fixes, we forget our bodies aren’t machines. You think a pill solves everything? Nah. You think the FDA cares? Nope. They’re too busy getting paid by Big Pharma. This is why I’m done trusting the system.
Rajni Jain
December 30, 2025 AT 15:48i read this and my heart went out to so many people i know who are scared to ask their doctors about pain. they just suffer because they’re afraid of being judged. thank you for saying this so clearly. you’re not alone. and you don’t have to take the risk. talk to your doctor. try the gel. move gently. you got this.
Sumler Luu
December 31, 2025 AT 10:26One thing I’d add: even topical NSAIDs aren’t 100% safe for everyone. I had a patient whose INR spiked after using diclofenac gel for six weeks. It’s minimal absorption, but still absorption. Always monitor. Always ask. Always be your own advocate.
sakshi nagpal
January 2, 2026 AT 07:51It's fascinating how we've created a medical culture where pain is seen as a problem to be eliminated, not a signal to be understood. Warfarin users are often left with few options because we prioritize convenience over safety. Perhaps the real issue isn't the drugs-it's our expectation that everything should be instantly fixable.
Sandeep Jain
January 4, 2026 AT 02:31my uncle took naproxen for his knee and ended up in the er with a bleed. they gave him 6 units of blood. he still doesn’t get why it happened. this post is a must read for anyone on warfarin. please share it with your family.
roger dalomba
January 6, 2026 AT 00:03Wow. A whole essay on why you shouldn’t take Advil. Groundbreaking. I’m sure the FDA will be issuing a press release any minute now.
Brittany Fuhs
January 6, 2026 AT 07:11Why do we let foreigners prescribe this stuff? In America, we know better. You think someone in India understands warfarin? Please. This is why our healthcare’s a mess. Use Tylenol. Or don’t. But don’t blame the system when you bleed out. It’s your fault.
Sophia Daniels
January 7, 2026 AT 22:24Let me tell you what happens when you ignore this: you wake up with a headache, think it’s just stress, then pass out on the bathroom floor with your pillow soaked in blood. No warning. No second chance. Just… gone. Your dog licks your face. Your cat jumps on the bed. And you’re just… cold. This isn’t a warning. It’s a funeral waiting to happen. Stop. Just. Stop.
Steven Destiny
January 9, 2026 AT 12:40Look, I get it. You’re scared. But don’t let fear paralyze you. Talk to your doctor. Get the PPI. Use the gel. Try PT. You can still live well. You just have to be smart. This isn’t the end of your life-it’s just a new chapter. And you’ve got this.
Fabio Raphael
January 10, 2026 AT 15:47What about CBD oil? I’ve heard some docs are starting to recommend it for chronic pain in anticoagulated patients. Any data on that?